KEY TAKEAWAYS:
- Low testosterone can cause symptoms such as fatigue, erectile dysfunction, and lack of energy, negatively impacting a person’s daily life and self-esteem.
- Diagnosing low testosterone involves checking laboratory tests and assessing other hormones that may affect testosterone levels.
- Treatment options for low testosterone include gels and injectable testosterone, which can have a significant positive impact on patients’ lives.
Dr. Amar J. Raval on Low Testosterone
Amar J. Raval, MD, is a urologist in Tampa, FL, specializing in the diagnosis and treatment of urological conditions, including low testosterone. Low testosterone can have a significant impact on an individual’s daily life and overall well-being. In this article, we will discuss the symptoms and treatment options for low testosterone, as advised by Dr. Raval.
Symptoms of Low Testosterone
Low testosterone, or hypogonadism, can present with a variety of symptoms that may negatively impact an individual’s quality of life. According to Dr. Raval, some of the common symptoms associated with low testosterone include:
- Fatigue
- Erectile dysfunction
- Lack of energy
These symptoms can interfere with a person’s daily activities, relationships, and self-esteem, making it crucial to seek appropriate treatment.
Diagnosing Low Testosterone
Dr. Raval explains that diagnosing low testosterone involves checking certain laboratory tests, including subsequent tests to confirm the low testosterone levels. In addition, other hormones that may affect testosterone levels are also assessed.
Treatment Options for Low Testosterone
Once low testosterone has been confirmed, Dr. Raval discusses various treatment options with patients. These options include:
- Gels: Topical testosterone gels are applied directly to the skin and absorbed through the skin’s surface. This method is convenient and relatively easy to administer, although it may cause skin irritation in some cases.
- Injectable testosterone: Testosterone injections are another treatment option for individuals with low testosterone. Injections provide a more direct route of administration, and dosing can be more easily controlled compared to gels.
The Impact of Testosterone Treatment on Daily Life
Dr. Raval emphasizes that testosterone treatment can have a dramatic effect on patients’ lives, including their sexual function, energy levels, productivity, and self-esteem. By addressing the underlying hormonal imbalance, patients can experience significant improvements in their overall well-being and quality of life.
Dr. Amar Raval and Advanced Urology Institute
Dr. Amar J. Raval is a urologist in Tampa, FL, who is dedicated to providing the best possible care for his patients. As a member of the Advanced Urology Institute, the largest urology practice in Florida, Dr. Raval works alongside a team of experienced urologists who share his commitment to excellence in patient care.
By offering comprehensive treatment options and personalized guidance for patients with low testosterone, the Advanced Urology Institute ensures that their patients receive the most advanced and effective treatments available in the field of urology.
TRANSCRIPTION:
My name is Amar J. Raval and I’m with Advanced Urology Institute. There’s plenty of patients who have low testosterone and want to know treatment options for that. They have fatigue, erectile dysfunction, lack of energy, and those can plague them in their daily lives. So generally now with the new screening guidelines with the AUA, we check certain labs. We need to show that they have low T on subsequent labs and we also check other hormones that may affect that. And those that are in need or can benefit from therapy, there’s gels as well as injectable testosterone that can be given to help them in that setting. I think it dramatically affects their lives. Their sexual lives, their energy, their being more productive throughout the day can affect relationships and even their self-esteem. So all of these are huge factors for them.
REFERENCES:
- “Low Testosterone (Low T): Causes, Symptoms & Treatment.” 2 Sep. 2022, https://my.clevelandclinic.org/health/diseases/15603-low-testosterone-male-hypogonadism.
- “Testosterone therapy: Potential benefits and risks as you age.” https://www.mayoclinic.org/healthy-lifestyle/sexual-health/in-depth/testosterone-therapy/art-20045728.
- “Low Testosterone: 12 Signs in Men – Healthline.” 26 May. 2022, https://www.healthline.com/health/low-testosterone/warning-signs.







 Obviously the heat is going to play a major role, a lot of it has to do with our diet unfortunately as well. [As with] an American diet, we just don’t eat very well, we’re all a little heavier and that also increases the risk of kidney stones as well.
Obviously the heat is going to play a major role, a lot of it has to do with our diet unfortunately as well. [As with] an American diet, we just don’t eat very well, we’re all a little heavier and that also increases the risk of kidney stones as well.

 Fortunately for men who suffer from BPH, medical progress is on their side. According to
Fortunately for men who suffer from BPH, medical progress is on their side. According to 
 Once an appointment is made with the urologist, doctor and patient can begin discussing symptoms and the diagnostic process. If the patient’s complaints are consistent with BPH, the urologist will proceed with a prostate exam. There are also other simple, non-invasive tests that can be completed at the urologist’s office that will indicate the patient’s urine flow and ability to empty his bladder. More sophisticated testing is available if additional data on the patient’s BPH issue is needed. For example, fiber optic scope evaluations give the urologist the most detailed picture of the patient’s BPH, which can then be used to devise the best treatment plan.
Once an appointment is made with the urologist, doctor and patient can begin discussing symptoms and the diagnostic process. If the patient’s complaints are consistent with BPH, the urologist will proceed with a prostate exam. There are also other simple, non-invasive tests that can be completed at the urologist’s office that will indicate the patient’s urine flow and ability to empty his bladder. More sophisticated testing is available if additional data on the patient’s BPH issue is needed. For example, fiber optic scope evaluations give the urologist the most detailed picture of the patient’s BPH, which can then be used to devise the best treatment plan.
 There is yet another exam called the
There is yet another exam called the 
 However, for some people, these methods are not enough to ensure they can live a healthy, fulfilling life. In these situations, surgical intervention is an option to correct overactive bladder problems.
However, for some people, these methods are not enough to ensure they can live a healthy, fulfilling life. In these situations, surgical intervention is an option to correct overactive bladder problems.
 Urologists will consider their patient’s health, age, and the type cancer when deciding how to proceed. For some cases, the best treatment is none at all. When a patient has
Urologists will consider their patient’s health, age, and the type cancer when deciding how to proceed. For some cases, the best treatment is none at all. When a patient has 
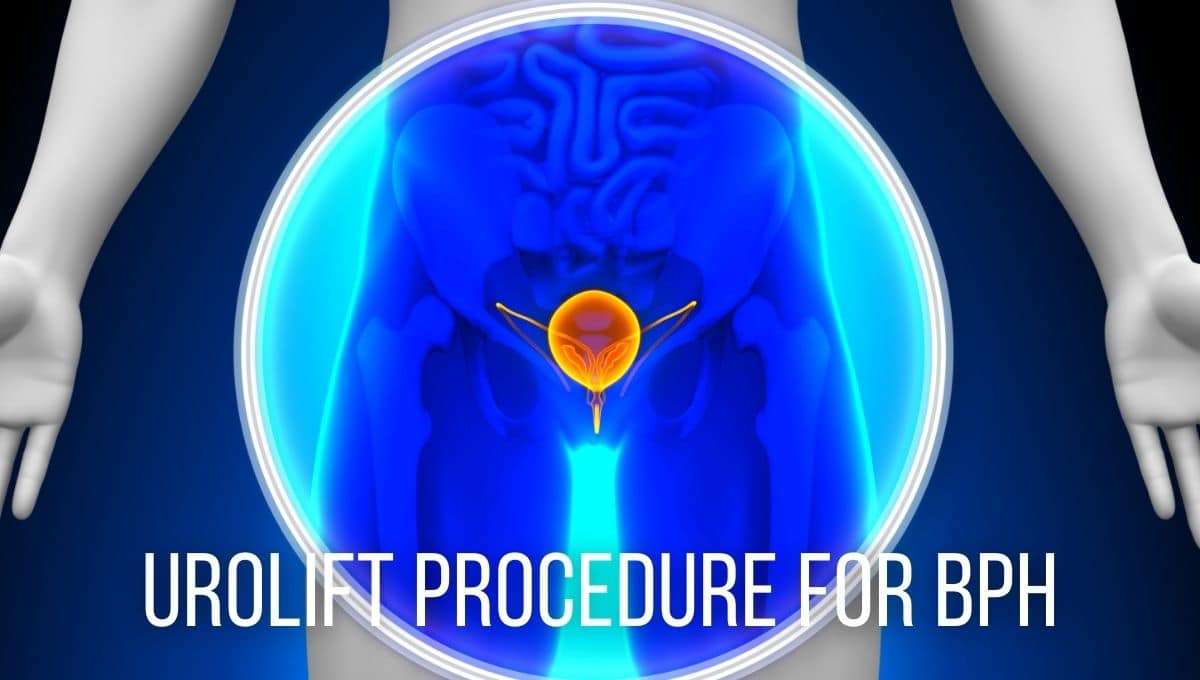
 For most men, the symptoms of an enlarging prostate include the slowing of their urine stream, pushing to urinate, and having to go to the bathroom frequently. Many men also have the feeling of not fully emptying their bladder after urination. In many cases, men will find that they need to wake up multiple times in the night to go to the bathroom.
For most men, the symptoms of an enlarging prostate include the slowing of their urine stream, pushing to urinate, and having to go to the bathroom frequently. Many men also have the feeling of not fully emptying their bladder after urination. In many cases, men will find that they need to wake up multiple times in the night to go to the bathroom.
 Urologists can usually diagnose
Urologists can usually diagnose