Dr. David DiPiazza, a urologist in New Port Richey, FL talks about the benefits of robotic surgery but also the potential for error.
Continue readingBrian Hale, MD Beyond Urology Exploring My Hobbies and Passions
When opting for a urologist, like Dr. Brian Hale, you will want one who understands the value of balance in everything, even beyond urology.
Continue readingDavid DiPiazza, MD: Advantages of Robotic Surgery
Dr. David DiPiazza, urologist in Trinity Duck Slough office in Florida talks about the advantages of robotic surgery in the field of urology.
Continue readingMedtronic’s InterStim Therapy for Incontinence with Dr. Ali Syed
Genetic Testing for Cancer Risk
What is MRI with Transrectal Ultrasound Fusion-Guided Prostate Biopsy
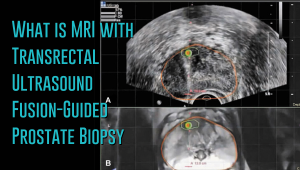 Prostate cancer has a new standard of care in MRI-guided fusion biopsy with transrectal ultrasound. While a prostate biopsy has been the only way to get a definitive diagnosis of prostate cancer, it has only been working if cancer cells are identified in the sample tissue. But in some cases, such as when the tumor occurs at the top surface of the prostate or other unusual locations, a biopsy may not give a correct diagnosis. For instance, the standard TRUS (transrectal ultrasound) guided biopsy in which tissue samples are collected from the prostate in a systematic pattern gives a negative result with tumors located in unusual areas of the prostate. About 15-20 percent of tumor locations can be missed by the biopsy needle.
Prostate cancer has a new standard of care in MRI-guided fusion biopsy with transrectal ultrasound. While a prostate biopsy has been the only way to get a definitive diagnosis of prostate cancer, it has only been working if cancer cells are identified in the sample tissue. But in some cases, such as when the tumor occurs at the top surface of the prostate or other unusual locations, a biopsy may not give a correct diagnosis. For instance, the standard TRUS (transrectal ultrasound) guided biopsy in which tissue samples are collected from the prostate in a systematic pattern gives a negative result with tumors located in unusual areas of the prostate. About 15-20 percent of tumor locations can be missed by the biopsy needle.
What makes the MRI-ultrasound fusion biopsy more definitive?
The MRI-ultrasound fusion approach is an improvement on the traditional 12-core TRUS, which involved taking biopsies from twelve prostate areas where the cancer is considered more likely to occur. With the TRUS biopsy, about 70 percent of men who have a negative biopsy result are not essentially free of the cancer. The MRI-ultrasound fusion technology blends the superior imaging capability of the high-definition multi-parametric (mp) MRI with real-time ultrasound imaging. There is better visualization of the suspicious areas of the prostate where the cancer may occur that may not be visible on ultrasound alone. The fusion-guided biopsy detects almost twice as many prostate cancers in all stages as the standard TRUS biopsy.
The ability of MRI-ultrasound fusion-guided biopsy to create a three-dimensional (3D) map of the prostate ensures that doctors are able to see the targeted areas of the prostate better and perform more precise biopsies. The technology uses a machine known as UroNav developed by Invivo, which is supplied with sophisticated software to produce super-detailed MRI images and fuse them with the ultrasound images generated by a transrectal probe administered on the patient in an outpatient setting. The resulting images enable the examining physician to direct biopsy needles with pinpoint accuracy and to easily access any lesions or suspicious areas revealed by MRI. The technology allows the urologist to hit the target spot more accurately and improves cancer detection rate. In fact, it is primarily used for men who have an ongoing suspicion of prostate cancer, such as those with consistently elevated PSA, but whose TRUS biopsy results are repeatedly negative.
Fewer biopsies, more accurate detection
The fusion-guided biopsy is a very targeted approach in which biopsies are performed only in highly suspicious areas of the prostate appearing in the MRI image. As a result, significantly fewer biopsies are done with the MRI-ultrasound fusion than with the traditional TRUS technique, minimizing the adverse effects that often accompany repeat biopsies. Multiple prostate biopsies can lead to complications such as bleeding, infection, urinary retention problems, sepsis or even death.
In spite of fewer biopsies, the MRI fusion approach increases the rate of detection of aggressive prostate cancer. The extensive MRI images obtained before the biopsy helps highlight both high-risk and intermediate-risk cancers often missed by traditional TRUS biopsy. With MRI-ultrasound fusion, the likelihood of detecting cancer increases as the grade of the tumor increases. The use of MRI fusion biopsy helps to avoid metastatic disease by finding cancer before it spreads to other areas of the body.
Improved cancer differentiation
Through MRI fusion, doctors are able to more accurately differentiate cancers that require treatment from the ones that should undergo watchful waiting (active surveillance). Fusion technology is able to show higher-risk cancers and does not highlight the insignificant low-grade tumors, making it less likely for urologic oncologists to over-treat indolent and low-grade cancers. A number of prostate cancers are low-grade, non-aggressive and do not cause problems at all and treating them through chemotherapy, radiotherapy or surgery can impair the quality of life or even cause death. MRI fusion effectively saves patients from the adverse effects of treating low-grade tumors. Fusion technology eliminates up to 50 percent of prostate cancer treatments that are unnecessarily administered on low-grade cancers.
At Advanced Urology Institute, we have adopted the MRI-ultrasound fusion biopsy and changed the way we screen, evaluate and diagnose prostate cancer. It has become our standard for detecting prostate cancer and we believe in the next few years it will be the gold standard for detecting the cancer. We are proud that it offers a higher detection rate, superior accuracy and reduces the rate of repeat biopsies — making our practice one of the best places for detection and monitoring of the cancer. It helps us deliver the best treatment outcomes for our patients.
If you think you are at high risk of prostate cancer or already have started experiencing some symptoms, let us show you how the precision of our high-definition MRI fusion machine, the expertise of our skilled physicians in MRI fusion biopsy and the know-how of our radiologists proficient in multi-parametric MRI imaging can help you. For more information on the treatment and diagnosis of prostate cancer, visit the “Advanced Urology Institute” site.
Becoming A Urologist with Dr David DiPiazza
Intriguing, inspiring and interesting, urology is a great profession for a person in love with solving problems, tackling embarrassing situations, saving lives and relating to the stories of humanity. As a urologist, you see people with awkward urine leaks, inability to get an erection, devastating genitourinary cancer and many other depressing and humiliating conditions every day. Fixing these issues and restoring sparkle, enthusiasm and joy to their lives is tremendously rewarding. It’s a unique position that also provides you with the opportunity of continuous learning and satisfaction. It’s an occupation I dreamed of as a child and which I now cherish as a doctor.
Path to Urology
When I completed my undergraduate studies at Cornell University’s prestigious Ivy College, achieving honors of cum laude, I opted to pursue a urology residency to specialize in a field with so many issues to be tackled but so few medical students turning to it.
For a six-year training span that took me to Princeton Medical Center, The Cancer Institute, New Jersey, and Robert Wood Johnson University Hospital, I honed my skills in all aspects of male and female urology, urologic oncology and robotic surgery. With this extensive training and experience I was able to achieve a double certification in 2006 by Female Pelvic Medicine and Reconstructive Surgery and the American Board of Urology. It took me just 5 years of practice to be honored by my peers for excellent work, being elected the Chief of Surgery at the Medical Center of Trinity, originally the Community Hospital.
Areas of Expertise
I routinely tackle the most common urological problems, such as kidney stones, urologic cancers, UTIs, urinary incontinence, enlarged prostate and overactive bladder. As an expert in no-needle, no-scalpel vasectomy, I also perform quite a number of vasectomies in my office. Likewise, because of my skill and experience in advanced laparoscopic technologies and da Vinci robotic I handle several cases of urogynecology and urologic oncology in Florida.
Some of the procedures I perform routinely include sacrocolpopexy (minimally invasive repair of vaginal prolapse), hysterectomy and sling procedures for urinary incontinence, cystectomy (bladder removal) in those with significant bladder cancer, nerve-sparing prostatectomy (prostate removal) for prostate cancer, nephrectomy (kidney removal) to treat kidney cancer, ureter repair and reconstruction in case of obstruction or injury, adrenalectomy (adrenal gland removal) and pyeloplasty (reconstruction of renal pelvis). I am also a robotic surgery instructor and an expert reviewer with C-SATS certification.
Job Satisfaction
As a urologist, the work hours are often long and I usually find myself in situations that are stressful. But to persevere through them and consistently provide safe, timely and effective remedies to those in great need is incredibly satisfying and keeps me going. The challenges just help bring out the best in me and make my job even more fulfilling. Urology is deeply fascinating as I am not just able to tackle embarrassing problems, but also to examine the urinary system and administer treatment with some of the most advanced and innovative technology.
There’s never a dull moment for a urologist as you see different kinds of people and sort out different issues every day, a guarantee that each day will bring some kind of excitement. You also get the opportunity to know these people, earn their trust and build very close, long-term relationships. I find it quite gratifying to care for patients with often devastating and humiliating issues and to see their situations improve.
Why Advanced Urology Institute
During my training years, I looked forward to an ideal workplace — one that would bring out the best of my talents, skills and experiences and empower me to provide the best possible care. And I found it in Advanced Urology Institute. At AUI, I have no administrative work to trouble me, so I spend most of my time caring for my patients and collaborating, innovating and researching for safe and effective solutions to my patients’ problems. And because AUI brings together a huge pool of skilled, creative, passionate and hard-working medical professionals, it makes it easier for me to perform at my best and to take my career to the heights I desire. I couldn’t have found a better workplace than AUI. For more information on the urological services at AUI, visit the “Advanced Urology Institute”site.