Explore the inspiring journeys of Drs. Selinger and Ramos, showcasing the profound impact of a dedicated career in urology.
Continue readingScott Sellinger, MD: Choosing Advanced Urology Institute – My Reasons and Vision
Choosing Advanced Urology Institute in Florida was obvious for Dr. Scott Sellinger in his unrelenting quest for quality in urological care.
Continue readingThe Enjoyment of Being a Urologist
Urology is a wonderful specialty, being at the same time a surgical and medical practice. It offers an interesting mix of work in both the office and the operating room.
“For many of us, we enjoy spending time in the operating room—after all, we are surgeons by trade,” says Dr. Scott B. Sellinger, FACS, a board-certified urologist at Advanced Urology Institute. “But for many of us, we also enjoy interactions with our patients in the office. I love to see my folks, especially the ones I’ve been seeing for the past 25 years. They come back every year and we can chat about all kinds of things.”
Interesting surgical techniques
While most urology patients are followed long-term with medical interventions, at least half of them are surgical patients. The subspecialty of urology offers great opportunities to practice the surgical side of the profession, which includes the hands-on application of the latest technology, such as robots and lasers. “I enjoy the surgical side of our profession, and urology offers innovative techniques and technology that makes surgical procedures even more interesting,” says Dr. Sellinger.
Long-term relationships
The opportunity to build lasting doctor-patient relationships makes urology gratifying.
“As a urologist, you get to care for the entire spectrum of age groups of patients, such as children with congenital problems and patients in their declining years, when a lot of urologic problems tend to set in.” says Dr. Sellinger. “I like the fact that I see different patients every day, delve into their emotional problems, and with empathy, provide the support and solutions they need. I also enjoy speaking with the patients I see every year for several years since every time they come in they have something great to share,” he adds.
Tackling embarrassing problems
Urology brings relief to patients with personal and sometimes embarrassing medical problems. Through surgery, medications or both, urologists resolve these issues and improve the quality of life of their patients, which is quite appealing.
“As a urologist, not only do I treat life-threatening conditions like cancer, I also improve the quality of life of patients by freeing them from sexual dysfunction or incontinence,” says Dr. Sellinger.
Great outcomes
Unlike some other specialties, the treatments offered by urologists often provide quick relief and good outcomes. In fact, most patients treated by urologists do well and get better.
“Nowadays, urology is quite advanced, and we have at our disposal medicines, surgery, and the combination of both treatments that render our patients improved soon after they interact with us,” says Dr. Sellinger. “So we feel satisfied and secure in the knowledge that we can solve most, if not all, of the urologic problems,” he adds.
Because of consistently great results, urologists are held in high regard by their patients, who are usually grateful for the care. In turn, this gives a kind of satisfaction to urologists.
“I am happy that I chose urology. I’m always filled with joy every time patients come back to thank me for what I’ve achieved for them,” says Dr. Sellinger. “If I were to start all over again, I would still choose to become a urologist.”
Personalized, compassionate care
Want to have your urological problem treated by an effective urologist? AUI is a medical group with a long history of providing comprehensive, high-quality care. The urologists at AUI find it a joy to work in an environment that brings out the best of their knowledge and experience for the benefit of their patients.
Whether you have kidney, urinary tract, prostate, pelvic or other urological needs, at AUI you will find a urologist who can deliver the right treatment for you. For more information on the diagnosis and treatment of urological conditions, visit the Advanced Urology Institute website.
Types of Prostate Cancer: What You Need to Know
Prostate cancer is a complex disease. It is not easy to predict how any particular prostate tumor will grow, or how rapidly it will spread to areas outside the prostate. After a prostate cancer diagnosis, your urologist will assess various factors to determine the level of risk associated with the disease. Understanding the risk level—low, intermediate or high—will help you and your doctor make decisions to achieve the best survival rate and quality of life.
Types of prostate cancer
While there are many types of prostate cancers, urologists first divide them into two categories—aggressive and indolent—to begin determining the best treatment.
1. Aggressive prostate cancer
 Aggressive prostate cancer is the type that grows rapidly, spreads fairly early, quickly and widely, and causes massive body damage. Since it spreads swiftly via secondary deposits, it quickly becomes advanced stage cancer and is very difficult to treat, particularly during the later stages.
Aggressive prostate cancer is the type that grows rapidly, spreads fairly early, quickly and widely, and causes massive body damage. Since it spreads swiftly via secondary deposits, it quickly becomes advanced stage cancer and is very difficult to treat, particularly during the later stages.
For aggressive high-risk prostate cancer, treatment is most effective when it begins while the tumor is still in its early stages. Without early treatment, the cells of the tumor remain highly active, multiplying rapidly. The tumor grows swiftly, spreads rapidly and causes widespread damage.
2. Indolent prostate cancer
Indolent prostate cancer is the type that grows very slowly and is unlikely to spread to areas outside the prostate. Therefore, it is a low-risk, low-volume tumor that can exist in the prostate for several years without causing significant problems. Even if left untreated, it is unlikely to spread outside the prostate; and if it spreads, it only does so slowly and locally.
How are high-risk and low-risk prostate tumors identified?
If you are diagnosed with prostate cancer, your doctor will monitor the disease periodically to see if it is growing and spreading. The primary way for monitoring the growth and spread of the tumor is the prostate-specific antigen (PSA) level in blood. PSA is produced by the prostate and reaches the bloodstream; but larger amounts of PSA in the bloodstream are usually a signal that the prostate is enlarged, infected or malignant.
For instance, the PSA doubling time—the time it takes for a patient’s PSA level to double—predicts how aggressive the cancer is. The faster the PSA level doubles, the more aggressive is the cancer. Likewise, the PSA velocity helps to predict the aggressiveness of a tumor. If the PSA level increases sharply, then the cancer is likely aggressive.
Urologists also use the Gleason score to detect how fast the cancer is growing and spreading. This score is obtained by grading cells in the tumor on the basis of how abnormal or normal the cells look under the microscope. The two most abnormal areas of the tumor are evaluated, each given a score from 1-5, and then the two numbers are added. The higher the score (typically 6 or more), the more aggressive the tumor.
While immediate treatment is called for with aggressive, high-risk tumors, a patient can live with an indolent, low-risk tumor for 20-30 years without the cancer causing any serious effects. For the slow growing tumor, we may recommend observation or a watchful waiting called active surveillance, where we monitor the growth and spread of the tumor without medical intervention.
At Advanced Urology Institute, we offer a wide range of treatment options for prostate cancer, including chemotherapy, hormone therapy, radiotherapy, and surgery. But before we can recommend any treatment, we try to determine the risk of advanced disease. For more information on the diagnosis and treatment of prostate cancer, visit the Advanced Urology Institute website.
Erectile Dysfunction Overview
Erectile dysfunction (male impotence) is a man’s inability to achieve or maintain an erection with enough firmness to have satisfying sex. Occasional erectile dysfunction (ED) is common and many men experience it when undergoing some form of stress. But frequent ED can be a sign of serious health, emotional or relationship problems that require the attention of a professional.
How common is erectile dysfunction?
Roughly 30 million men in the United States have problems achieving or maintaining an erection. The frequency of ED increases with age, affecting only 5-40% of men in their 40’s and up to 50-80% of men over 70 years. However, while the risk of ED increases with age, the condition is not an inevitable consequence of aging. Good health is the key to a lifetime of good sexual function.
Who is at risk of erectile dysfunction?
 Apart from occurring frequently among the elderly, ED is often a consequence of poor emotional and physical health. It is common in men with high cholesterol, diabetes, obesity, cardiovascular disease, hypertension, prostate disease, anxiety, damage from surgery or cancer, injuries, stress, depression, performance anxiety, relationship problems, alcohol use, smoking, and drug use. Typically, ED is caused by vascular disease (such as atherosclerosis) that prevents blood supply to the penis, a neurological disorder (like multiple sclerosis) that cuts transmission of nerve impulses to the penis, chronic medical disorders such as Peyronie’s disease, stroke and diabetes, trauma, and operations for bladder, colon and prostate cancer which may affect blood supply to the penis. These risk factors may work singly or in combination.
Apart from occurring frequently among the elderly, ED is often a consequence of poor emotional and physical health. It is common in men with high cholesterol, diabetes, obesity, cardiovascular disease, hypertension, prostate disease, anxiety, damage from surgery or cancer, injuries, stress, depression, performance anxiety, relationship problems, alcohol use, smoking, and drug use. Typically, ED is caused by vascular disease (such as atherosclerosis) that prevents blood supply to the penis, a neurological disorder (like multiple sclerosis) that cuts transmission of nerve impulses to the penis, chronic medical disorders such as Peyronie’s disease, stroke and diabetes, trauma, and operations for bladder, colon and prostate cancer which may affect blood supply to the penis. These risk factors may work singly or in combination.
How is erectile dysfunction treated?
When you visit a urologist, the first step in the diagnosis of the problem is a thorough sexual, medical and psychosocial history. Physical examination with emphasis on the genitourinary, neurologic and vascular systems is performed. From the information gathered, the urologist may request hormone tests (testosterone, luteinizing hormone, and thyroid – stimulating hormone, prolactin and serum hormone-binding globulin), urinalysis, PSA (prostate-specific antigen), lipid profile, and serum chemistry. Functional tests such as prostaglandin E1 injection, formal neurologic testing, nocturnal penile tumescence testing and biothesiometry may be requested, together with imaging studies such as transrectal, testes and penile ultrasonography and angiography.
If erectile dysfunction is diagnosed, the doctor may recommend treatment depending on the cause and severity of the condition. For instance, the urologist may recommend sexual counseling when no organic causes can be established for the problem. Oral medications such as sildenafil, vardenafil, tadalafil or avanafil may be offered to relieve the problem. But for those not responding to oral medicines, the urologist may inject, implant or direct the topical application of drugs such as alprostadil, phentolamine or papaverine. In some cases, an external vacuum or constriction device may be recommended while for other patients hormone replacement therapy may be used to treat severe hypogonadism (lower-than-normal testosterone). Alternatively, the urologist may opt for surgery through procedures such as revascularization, placement of penile implant or surgical correction of venous outflow.
How is erectile dysfunction prevented?
- Eat a healthy, balanced diet that avoids saturated fats and increases the intake of vegetables, fruits and whole grains.
- Reduce cholesterol levels through exercise, medication and diet.
- Maintain a healthy body weight.
- Exercise regularly.
- Seek prompt treatment or professional help for conditions such as stress, depression, hypertension, heart disease and diabetes.
At Advanced Urology Institute, we recognize that effective treatment of erectile dysfunction involves a proper determination of the underlying cause and a frank discussion of both medical and non-medical options. This is why we have assembled an accomplished team of physicians, state-of-the-art facilities and a patient-centered system that responds to the unique needs of each patient. If you are experiencing a urological problem, make an appointment today. For more information, visit the Advanced Urology Institute website.
Vasectomy: Easy Safe Effective Birth Control
As a permanent method of birth control, vasectomy has been around for decades with good results. Today it is performed as a routine procedure with over 500,000 operations done in the United States each year.
During the procedure, the vas deferens (the duct that carries sperm from the testicles to the urethra) is cut or blocked to prevent sperm from being released during ejaculation. Sperm must travel from a man’s testicles to the urethra for pregnancy to occur during sexual intercourse, and blocking this passage is what makes vasectomy an effective method of birth control.
How is a vasectomy performed?
 A vasectomy is an outpatient procedure that must be performed in a medical facility or in a doctor’s office. In one technique, the urologist makes two small incisions on either side of the scrotum in order to gain access to the vas deferens. In another technique, the urologist makes one small incision to access both tubes. After accessing the tubes, the doctor cuts and seals them and then adds stitches if necessary. Doctors perform vasectomy under local anesthesia, making it as painless as possible. The procedure takes 10-20 minutes and the patient is free to go home immediately.
A vasectomy is an outpatient procedure that must be performed in a medical facility or in a doctor’s office. In one technique, the urologist makes two small incisions on either side of the scrotum in order to gain access to the vas deferens. In another technique, the urologist makes one small incision to access both tubes. After accessing the tubes, the doctor cuts and seals them and then adds stitches if necessary. Doctors perform vasectomy under local anesthesia, making it as painless as possible. The procedure takes 10-20 minutes and the patient is free to go home immediately.
Recovery from the operation is easy. Your doctor will give you clear instructions which, if followed, will allow you to get back to normal in a few days. To ensure a quick recovery, you will need to apply cold packs to the area for 12-48 hours and lie on your back as much as possible. Wearing comfortable underwear or a jockstrap will protect the area. It is common to have mild discomfort, bruising and swelling of the scrotum for a few days after a vasectomy. In case of persistent and considerable pain, contact your doctor for advice. Unless your job is strenuous, you can return to work in 1-2 days. However, you must avoid heavy lifting for at least a week to avoid aggravating the wound.
How effective is vasectomy?
Vasectomy boasts of a better success rate than even the most effective forms of female contraception. The chance that a vasectomy fails (and a man impregnates his partner after the operation) is anywhere from 0.3% to 9% in the first six months after surgery. This is usually because it will take a few months for semen to be fully without sperm. Doctors suggest using another method of birth control such as condoms until follow-up analysis of semen shows zero sperm. But after this initial period, the failure risk of vasectomy drops to between 0.04% and 0.08% (about 1 in 2000). In comparison, the failure rate of intra-uterine device (IUD) is 0.2% to 0.8% while that of tubal ligation is nearly 1% during the first year after the procedure. Therefore, vasectomy is not only the best birth control method for men, but also one of the best overall.
Easy, safe and effective birth control
Vasectomy is a safe and low-risk way a man can take on the medical responsibilities of family planning. Whether you want to commit to a child-free life or do not want any more children, vasectomy is a long-term, discreet, 10-20 minute procedure with no danger to your hormonal balance and sex life. It is safer than common forms of contraception for women and recovery is quick and easy. Although this procedure should always be considered a permanent change, the success rate for vasectomy reversals is between 40% to 90% depending on how the original procedure was performed. If you decide that you do not want any more children, this procedure is worth discussing with your doctor. For more information, visit the Advanced Urology Institute website.
Symptoms of Kidney Stones -Beyond the Basics
Kidney stones occur when hard deposits (minerals and salts) form inside the kidney. They vary in size and may travel to other parts of the urinary tract. While small stones may not produce any symptoms, some people complain of severe pain in different parts of the body. The excruciating pain can be likened to that of childbirth. Here is a quick guide on common symptoms of kidney stones.
1. Urge to urinate or frequent urination
Most people with kidney stones feel the urge to urinate. However, this will depend on where the stone is located. Those that are close to the bladder can irritate the walls and make the patient feel an urgent need to use the bathroom. These contractions may even occur when the bladder is empty. Keep in mind that unless the stone has moved to the urethra, there is no trouble when urinating.
2. Pain in the groin, back or side
Patients who experience pain around the groin or the lower abdomen may need a diagnosis for kidney stones. The pain also can occur under the rib cage or on the back side. It starts as a dull ache that escalates to sharp wincing pain. And it’s very episodic – it can be severe one minute and then completely subsides. The pain may be mild or barely noticeable. The patient may need to seek medical attention if the pain is very intense.
3. Nausea and vomiting
These two symptoms occur when the stones interrupt the flow of urine. It’s worth mentioning that stretching of the kidneys can cause gastrointestinal upset. And the worst part is that this pain does not subside even after making changes in body position. When patients vomit, they get dehydrated so additional fluids are recommended.
4. Blood in the urine
In advanced stages, a kidney stone can cause blood in the urine. The blood is only visible with dipstick testing or when examined with a microscope. People who spot pink or reddish urine should see a urologist immediately. Sometimes the urine may look like tea. This could be an underlying symptom to a more serious condition.
5. Fever
While this is not a common symptom for kidney stones, it occurs when patients have an infection in the problem area. According to experts, fever can occur when the stones block the flow of urine, which could be an emergency situation. And because the antibiotics can’t penetrate to an obstructed kidney, the obstruction must be relieved. Fortunately some stones may pass on their own without treatment.
Need the services of a urologist? Visit Advanced Urology Institute for professional treatment. Here you’ll find Dr. David Burday and other practicing urologists. They will do their best to put you at ease. For more information on treatment of kidney stones and other urological problems, visit our “Advanced Urology Institute” site.
Robotic Assisted Laparoscopic Radical Prostatectomy
Robotic-Assisted Laparoscopic Prostatectomy is a viable option for treating prostate cancer. It is a minimally invasive method for accessing both seminal vesicles and prostate glands during treatment of prostate cancer. Robotic prostatectomy is performed by an experienced surgical team with the help of advanced surgical robotic technology.
What is Robotic-Assisted Radical Prostatectomy?
Robotic prostatectomy involves the use of a laparoscopic system and Robotic Surgery System called da Vinci® Surgical System. This is a sophisticated robotic system designed to enable the surgeons to operate with enhanced vision, precision and control.
With the help of the surgical system, it is possible to pass miniaturized robotic instruments through keyhole incisions and remove the prostate and other nearby tissues with greater accuracy. During a robotic-assisted radical prostatectomy, it is able to create an incision that extends from the belly button to the pubic bone.
In the Robotic-Assisted Laparoscopic Radical-Prostatectomy, an image processing machine and a three-dimensional endoscope are used to achieve a clear and magnified view of structures around the prostate gland. This makes it possible to extract affected parts with optimal preservation of critical body parts such as blood vessels, nerves and muscles.
During the procedure, the surgeon operates the surgical system using a computer console that enables him to control tiny flexible instruments. This makes it possible to achieve higher precision and mobility. The whole process is done without the surgeon’s hand entering the area of the surgery in the patient’s body.
Advantages of Robotic-Assisted Laparoscopic-Radical Prostatectomy:
Robotic prostatectomy has some benefits compared to the traditional open surgical methods. Here are some of the advantages:
- Less pain
- Less loss of blood during the operation
- Shorter stay in the hospital.
Possible risks of Robotic-Assisted Prostatectomy:
The following are possible risks associated with the Robotic Assisted Laparoscopic-Radical Prostatectomy, although they are very unlikely:
- Damage to adjacent tissue or organ
- Infection of surgical site
- Bleeding
Laparoscopic Radical Prostatectomy:
As with all surgical methods, the robotic-assisted radical prostatectomy has a number of potential side effects, which include:
- Urinary incontinence or inability to control urine. However, this problem will reduce over time.
- Erectile dysfunction or impotence: Depending on the age of the patient, erectile function is likely to be affected.
Advanced Urology Institute is a patient-centered institute that works to minimize the possible side effects of a procedure. They research and partner with the best board-certified urologists, among them Dr. David Burday, to make sure that patients have a good experience during the operation and heal well afterward. For further information, visit the “Advanced Urology Institute” website.
What is MRI with Transrectal Ultrasound Fusion-Guided Prostate Biopsy
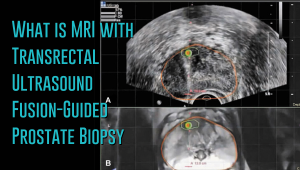 Prostate cancer has a new standard of care in MRI-guided fusion biopsy with transrectal ultrasound. While a prostate biopsy has been the only way to get a definitive diagnosis of prostate cancer, it has only been working if cancer cells are identified in the sample tissue. But in some cases, such as when the tumor occurs at the top surface of the prostate or other unusual locations, a biopsy may not give a correct diagnosis. For instance, the standard TRUS (transrectal ultrasound) guided biopsy in which tissue samples are collected from the prostate in a systematic pattern gives a negative result with tumors located in unusual areas of the prostate. About 15-20 percent of tumor locations can be missed by the biopsy needle.
Prostate cancer has a new standard of care in MRI-guided fusion biopsy with transrectal ultrasound. While a prostate biopsy has been the only way to get a definitive diagnosis of prostate cancer, it has only been working if cancer cells are identified in the sample tissue. But in some cases, such as when the tumor occurs at the top surface of the prostate or other unusual locations, a biopsy may not give a correct diagnosis. For instance, the standard TRUS (transrectal ultrasound) guided biopsy in which tissue samples are collected from the prostate in a systematic pattern gives a negative result with tumors located in unusual areas of the prostate. About 15-20 percent of tumor locations can be missed by the biopsy needle.
What makes the MRI-ultrasound fusion biopsy more definitive?
The MRI-ultrasound fusion approach is an improvement on the traditional 12-core TRUS, which involved taking biopsies from twelve prostate areas where the cancer is considered more likely to occur. With the TRUS biopsy, about 70 percent of men who have a negative biopsy result are not essentially free of the cancer. The MRI-ultrasound fusion technology blends the superior imaging capability of the high-definition multi-parametric (mp) MRI with real-time ultrasound imaging. There is better visualization of the suspicious areas of the prostate where the cancer may occur that may not be visible on ultrasound alone. The fusion-guided biopsy detects almost twice as many prostate cancers in all stages as the standard TRUS biopsy.
The ability of MRI-ultrasound fusion-guided biopsy to create a three-dimensional (3D) map of the prostate ensures that doctors are able to see the targeted areas of the prostate better and perform more precise biopsies. The technology uses a machine known as UroNav developed by Invivo, which is supplied with sophisticated software to produce super-detailed MRI images and fuse them with the ultrasound images generated by a transrectal probe administered on the patient in an outpatient setting. The resulting images enable the examining physician to direct biopsy needles with pinpoint accuracy and to easily access any lesions or suspicious areas revealed by MRI. The technology allows the urologist to hit the target spot more accurately and improves cancer detection rate. In fact, it is primarily used for men who have an ongoing suspicion of prostate cancer, such as those with consistently elevated PSA, but whose TRUS biopsy results are repeatedly negative.
Fewer biopsies, more accurate detection
The fusion-guided biopsy is a very targeted approach in which biopsies are performed only in highly suspicious areas of the prostate appearing in the MRI image. As a result, significantly fewer biopsies are done with the MRI-ultrasound fusion than with the traditional TRUS technique, minimizing the adverse effects that often accompany repeat biopsies. Multiple prostate biopsies can lead to complications such as bleeding, infection, urinary retention problems, sepsis or even death.
In spite of fewer biopsies, the MRI fusion approach increases the rate of detection of aggressive prostate cancer. The extensive MRI images obtained before the biopsy helps highlight both high-risk and intermediate-risk cancers often missed by traditional TRUS biopsy. With MRI-ultrasound fusion, the likelihood of detecting cancer increases as the grade of the tumor increases. The use of MRI fusion biopsy helps to avoid metastatic disease by finding cancer before it spreads to other areas of the body.
Improved cancer differentiation
Through MRI fusion, doctors are able to more accurately differentiate cancers that require treatment from the ones that should undergo watchful waiting (active surveillance). Fusion technology is able to show higher-risk cancers and does not highlight the insignificant low-grade tumors, making it less likely for urologic oncologists to over-treat indolent and low-grade cancers. A number of prostate cancers are low-grade, non-aggressive and do not cause problems at all and treating them through chemotherapy, radiotherapy or surgery can impair the quality of life or even cause death. MRI fusion effectively saves patients from the adverse effects of treating low-grade tumors. Fusion technology eliminates up to 50 percent of prostate cancer treatments that are unnecessarily administered on low-grade cancers.
At Advanced Urology Institute, we have adopted the MRI-ultrasound fusion biopsy and changed the way we screen, evaluate and diagnose prostate cancer. It has become our standard for detecting prostate cancer and we believe in the next few years it will be the gold standard for detecting the cancer. We are proud that it offers a higher detection rate, superior accuracy and reduces the rate of repeat biopsies — making our practice one of the best places for detection and monitoring of the cancer. It helps us deliver the best treatment outcomes for our patients.
If you think you are at high risk of prostate cancer or already have started experiencing some symptoms, let us show you how the precision of our high-definition MRI fusion machine, the expertise of our skilled physicians in MRI fusion biopsy and the know-how of our radiologists proficient in multi-parametric MRI imaging can help you. For more information on the treatment and diagnosis of prostate cancer, visit the “Advanced Urology Institute” site.
Common Cause of Kidney Stones
Kidney stones are a common condition in the United States affecting about 9 percent of Americans. Every year, roughly 500,000 patients are admitted into emergency rooms because of kidney stones. While the prevalence of the condition has risen over the years, increasing from 1-in-20 people in 1994 to 1-in-11 in 2012, the trend is expected to continue, both in broader geographic coverage and in greater numbers due to extreme temperatures associated with climate change. Higher temperature leads to dehydration, which in turn contributes to increased concentrations of dissolved salts and other substances in urine. When urine is super-saturated, it allows kidney stones to develop.
Low Urine Volume
The risk of kidney stones increases with decrease in urine volume. Caused by poor fluid intake or fluid loss (dehydration) due to hard exercise, living or working in a hot place, low urine volume means there is less fluid available to dissolve salts and other urine constituents. In turn, the urine becomes darker in color, more concentrated and easily forms stones. In fact, a urine volume below 1 liter per day is associated with 10 percent of all recurrent kidney stones while urine volume below 1.5 liters per day is linked with the formation of many recurrent and first-time kidney stones. Low urine volume due to chronic dehydration, defined as a history of prolonged exposure to heat, is the main cause of 20 percent of all incidents of kidney stones.
Effect of Warmer Temperatures
Cases of kidney stones typically increase shortly after episodes of hot weather, hitting a peak within three days of exposure to extreme heat. According to a recent study published in the Environmental Health Perspectives, daily increase in average temperatures leads to increased risk of formation of kidney stones. Another study published in 2008 by the National Academy of Sciences also reported that about 70 percent of Americans are under high risk of kidney stones due to warmer temperatures compared to just 40 percent of Americans at risk in 2000. The number of cases of heat-related kidney stones is projected to increase to up to 2.2 million by 2050.
Hidden Risk
Increase in ambient temperatures results in increased fluid losses through the skin. As more water is lost in sweat and less in urine, salts can build up in urine resulting in stones. Even in cold weather, dehydration occurs in the warm and dry indoor air without being noticed. And since dehydration often occurs without being noticed, it is a bigger factor in kidney stone formation in many patients. For instance, in drier climates, people lose a lot of water through sweat without realizing it and face a greater risk of kidney stone formation.
Are you or your loved one suffering from the symptoms of kidney stones? Would you like to receive world-class, safe, prompt and effective treatment for kidney stones? Or are you looking for the most comprehensive and accurate information on prevention, diagnosis and treatment of kidney stones? Then Advanced Urology Institute is the right place for you. At AUI, we offer patient-friendly and multidisciplinary urology services for a wide range of problems including kidney stones. For more information, visit the “Advanced Urology Institute” site.
Vasectomy: Easy, Safe, and Effective Birth Control
Vasectomy is a common form of birth control. More than 50 million men have undergone the procedure worldwide. In the United States, around 500,000 men get a vasectomy each year. Vasectomy is an easy, safe and effective surgical procedure carried out in a clinic, doctor’s office or hospital. The outpatient procedure takes 10-20 minutes and the patient can go back home on the same day. While it is still the fourth most preferred method of contraception after oral pills, condoms and tubal ligation, it is one of the cheapest, safest and most effective family planning options.
Vasectomy Procedure
During a vasectomy, the small tubes of the scrotum that transport sperm are blocked or cut off to prevent sperm from leaving the body and causing pregnancy. The name vasectomy comes from the vas deferens, the scrotal tubes that are blocked or cut off during the procedure. Vasectomy is intended for permanent sterilization, so while it can be reversed, only those who are sure they no longer want more children should undergo the procedure.
There are two common vasectomy techniques: the no-cut (no-scalpel) method and the incision method. No-scalpel technique is a lower-risk procedure that minimizes the chance of infection and complications while also taking less time to heal. Nevertheless, whatever method is used, vasectomy is a quick procedure performed with local anesthesia or IV sedation, depending on the patient’s condition and surgeon’s preferences. After numbing, one or two small incisions are used to access the vas deferens so they can be clamped, sealed or cut to disrupt sperm flow. The procedure is performed on both sides.
Recovery from vasectomy
Recovery time after vasectomy varies, but most men are able to return to normal physical activity in 2-3 days. Recovery is quite easy as the patient is able to go home soon after the procedure, rest, apply ice packs for 24-48 hours, watch football over the weekend and be able to resume work the following week. However, it is important to notify your doctor of any severe bruising, swelling, fever, pus or chills. These may indicate internal bleeding or infection and should be dealt with appropriately.
Safety and efficacy
Vasectomy is a highly effective method of preventing pregnancy, guaranteeing almost 100 percent efficacy. It is a safe and low-risk procedure, with just about 1 percent of men reporting side effects such as infection, bleeding and pain. Compared to tubal ligation, vasectomy is faster, less painful and has fewer potential complications. Vasectomy does not significantly change the amount of semen as only sperm will be absent from the ejaculate. It also does not change the way a man ejaculates or feels when having orgasm, so your sex life will remain the same except there will be no worry about pregnancy.
At Advanced Urology Institute, we use the most up-to-date no-scalpel techniques to perform vasectomy and vasectomy reversal quickly, painlessly and effectively. We take great care to review the medical history of every patient, evaluate and counsel our patients, answer all patient questions and ensure that only the right candidates undergo the procedure. We also deliver a safe and effective procedure through a patient-centered, multidisciplinary approach that guarantees the best services for all our patients. At AUI, your health is our number one priority. For more information on vasectomy and vasectomy reversal, visit the “Advanced Urology Institute” site.
Robotic Technology in Urology: Da Vinci Robotic Prostatectomy
Urology has always been one of the leading medical specialties in the adoption and application of the latest cutting-edge technologies. For many decades urology has been one of the areas of medicine that has often readily embraced new technologies and incorporated them into everyday practice for the benefit of patients. Urology was the first medical field to espouse and use scopes for various procedures. And then with the invention of robotic systems, urologists quickly adopted and integrated the da Vinci system in their practices, using it for prostate surgery and making the da Vinci prostatectomy one of the first mainstream
surgical procedures to be performed using robotic technology.
Influence of robotic surgical systems
The introduction of robotic systems in urology has quickly enabled urologists to overcome the limitations of open prostatectomy (traditional laparoscopy) such as limited instrument movement, difficult suturing, complex reconstruction and two-dimensional vision. Likewise, the introduction and quick assimilation of robotic technology has helped to solve the problem of surgeon fatigue in laparoscopic urology. Robotic systems have enabled urologists to perform complex reconstruction and dissection in less than 2 hours delivering excellent outcomes.
Overcoming limitations of open prostatectomy
Before the emergence of robotic surgical systems, men suffering from prostate cancer had very few treatment options. The principal surgical option available was open radical prostatectomy, a procedure that involved large incisions and serious post-operative side effects. For example, when using open prostatectomy, the removal of the entire cancerous prostate resulted in increased risk of post-operative infections, excessive blood loss, considerable pain and longer hospital stays. Open prostatectomy also may lead to loss of sexual function and bladder control due to cutting of the delicate nerve plexus around the prostate. The da Vinci robotic surgery is a minimally invasive procedure that uses smaller incisions, reduces blood loss and ensures a shorter hospital stay, making things better for the patient.
Utmost precision, great outcomes
The intuitive nature of the movement of robotic instruments results in highly precise, accurate, effective and safe prostatectomy. While laparoscopic surgery’s precision is reduced by the fulcrum effect (movement of the instrument tip in the direction opposite to the surgeon’s hands), the da Vinci robotic system has no fulcrum effect, offers three-dimensional visualization, boosts degrees of freedom, eliminates tremor, reduces fatigue and provides motion scaling and ergonomic positioning. Robotic surgery is a remote controlled process in which the surgeon’s movements are precisely translated through sensitive fibers to the instrument’s tip. When applied in prostatectomy, robotic systems have been found to offer several advantages over traditional laparoscopic surgery, including minimal scarring, diminished risk of complications, clinically superior results and quicker recovery.
State-of-the-art prostatectomy at Advanced Urology Institute
Want to be treated by a highly trained and experienced team of surgeons, technicians and nurses? At Advanced Urology Institute, we have urologists who are specialists in robot-assisted surgery for prostate cancer and other urological conditions. We perform dozens of surgical procedures every month using the da Vinci robotic system. This minimally invasive, high-precision robotic technology delivers great results with complex and delicate surgeries such as prostatectomies, where the target site is surrounded and confined by the nerves regulating erectile function and urinary flow. At AUI, we use the robotic system as an exacting tool to avoid damaging these nerves, shorten recovery time and ensure quick return to normal activities.
For more information on exceptional, world-class treatment using robotic technology, visit the “Advanced Urology Institute” site.
Kidney Stones: Causes, Symptoms, and Treatments
When there is inadequate liquid to dilute salts and waste chemicals found in urine, hard masses called kidney stones may form in the kidneys. The stones can form in one or both kidneys and may vary in size, ranging from a tiny sugar crystal to a large golf ball. While kidney stones are hard to notice, a stone can be large enough to cause blockage or severe pain, particularly when it enters into one of the ureters. Kidney stones are a common condition in the United States, affecting up to 9 percent of the population and sending more than 500,000 people to emergency rooms every year.
What are the symptoms of kidney stones?
While very small kidney stones may just pass through the urinary tract without causing symptoms, a majority of people who seek medical care for the condition do so because of severe pain on the flank, which may extend to the belly, groin or back. The movement of kidney stones through the urinary tract also may cause extreme pain that does not go away, painful urination, blood in urine, chills, fever, nausea and vomiting. When experiencing such symptoms, it is important to see a doctor as soon as possible for prompt medical attention.
Causes of Kidney Stones
Kidney stones occur when there is inadequate liquid to dilute the waste chemicals found in urine, such as oxalate, calcium and phosphorous. When not properly diluted, the waste chemicals get more concentrated and form crystals. The most frequent type of stones is calcium oxalate crystals. While there are many factors that can trigger the formation of kidney stones, including what you drink and eat and chronic medical conditions, the most common cause is dehydration. For instance, people living in hot climates are more likely to lose a lot of water in sweat, resulting in limited amounts of fluid available to dilute urine. The frequently high concentration of urine in such people can trigger kidney stones.
Diagnosing Kidney Stones
Kidney stones are often diagnosed once they have caused obvious symptoms, usually severe pain. The pain is typically so severe that it can send patients to emergency rooms where a range of tests may be conducted to uncover the stones. Apart from the symptoms, kidney stones are diagnosed using tests such as X-rays, CT scan, urinalysis and ultrasound. Blood tests to determine the levels of various minerals involved in stone formation also can unearth kidney stones.
Treatment of Kidney Stones
For small stones, no treatment is necessary. You may only need to take pain medications and wait for the stones to pass out. A stone that is 5mm (1/5 inch) or smaller has a 90 percent chance of passing without intervention while one between 5-10mm has a 50 percent chance of passing. To increase the chance of a stone passing on its own, it is important to drink a lot of fluid every day, such as 8-10 glasses of water daily. A stone that is larger than 10mm may not pass on its own and may require either a non-invasive or invasive treatment to remove it.
Prescription medications may be used to facilitate the passage of some stones that do not pass on their own. For example, alpha-blockers can be used to relax the walls of the ureters and widen the passages to allow the stones to move out easily. Certain medications also may be used to stop the formation of new stones.
Apart from using drugs, the surgeon can pass a special instrument called the ureteroscope through the urinary tract to reach the stone’s location. The surgeon then applies laser energy to break the stone into smaller fragments and remove them through the tube. The procedure is called ureteroscopy and it does not require incisions.
Another commonly used treatment for kidney stones is extracorporeal shock-wave lithotripsy (ESWL). This treatment is ideal for very large stones or for stones that have blocked the urinary tract. During shock wave lithotripsy, the surgeon uses a machine that generates strong vibrations (called shock waves) to break large stones into smaller pieces that can pass out through the urinary tract. However, for kidney stones that are extremely large, the surgeon may need to conduct a surgical operation to remove them.
A lot of technology is currently available to help diagnose, treat and manage kidney stones. The technologies are safe and effective, relieving the symptoms of kidney stones without causing problems to the patients. So if you are experiencing symptoms of kidney stones, visit your doctor as soon as possible to benefit from these latest technologies and get the necessary relief. You do not have to live with a problem whose solution exists. For more information on the diagnosis and treatment of kidney stones, visit the “Advanced Urology Institute” site.
Satisfactions of Being a Urologist – Dr. Scott B. Sellinger
When the term urology is mentioned, what comes to mind for many people is urine. But urology is a really huge medical field. It covers the diagnosis, treatment and management of a wide range of conditions affecting the female and male urinary tract and upsetting the male reproductive system. It is a dedicated medical field with highly trained and skilled specialist doctors called urologists.
“Urology is a massive field,” affirms Dr. Scott B. Sellinger of Advanced Urology Institute. “It is incredible the many problems we deal with. And when you have operated and developed worthwhile relationships with your patients, you go home every day feeling satisfied with your work. It is a truly exciting specialty.”
Problems resolved by urologists
Urology covers a broad spectrum of medical disorders affecting the ureters, kidneys, bladder, prostate, urethra, testis, epididymis, scrotum, penis and seminal vesicle. The most common conditions that urologists see are ejaculation problems, urinary incontinence, erectile dysfunction, cryptorchidism (undescended testes), vasectomy, vesicoureteral reflux, urinary tract infections and cancers of the kidneys, prostate, penis, testicles and bladder.
“As a urologist at Advanced Urology Institute, it is nice to come to work each day and look forward to fixing a female or male problem,” says Sellinger. “Urology is very unique because you work with the patients throughout the treatment cycle, right from diagnosis, treatment and recovery, so you get great satisfaction from seeing people recover and get on with their lives.”.
“While some specialists only diagnose but not treat the conditions and others just treat but are not involved in the entire disease management cycle, urologists are in the thick of it,” Sellinger explains. “I believe urology is the best-crafted medical field because you see everything as it occurs. It is gratifying.”
A hands-on field
“I love urology because I am a hands-on person,” says Sellinger. “In this field you physically do something and then see the results. I draw a lot of satisfaction from this.”
He adds, “The results are generally great in urology. In fact, many people with serious urological problems such as bladder and kidney cancers achieve great outcomes after our interventions.”
The work is very rewarding for the urologist too. “When you operate on people and they recover from their disorders and get on with life, it is fulfilling,” Sellinger notes. “I really feel happy about improving the quality of other people’s lives and relieving their pain.”
Personalized attention
In urology, each patient has different needs. It calls for a personalized approach to every patient. The urologist must take into account the factors presented by each patient, break down the needs and concerns, and then modify the consultations, diagnosis, treatment and follow-up interventions to meet the unique needs of the individual.
“The entire process of tackling urological problems is both challenging and thrilling,” says Sellinger. “Each case is unique and every patient requires a listening ear. So when you deal with a patient warmly and candidly, formulate effective treatment plans and then see positive results, the entire process brings indescribable joy, peace and satisfaction to the urologist.”.
Urologists also spend their time educating patients and the general public on preventive measures for various urological problems. For instance, they speak with men on when to go for screening for prostate cancer, alleviate fears about the risk factors and advise those diagnosed with the cancer on how to live positively with it.
“As urologists, we help relieve pain and distress and improve the quality of lives of men and women plagued by urological problems,” he explains. “We educate people on how to prevent some of these problems, encourage them to seek help early enough and administer treatments to help them recover. Many times, the results are great and satisfying.”
At Advanced Urology Institute, there is a big pool of experienced, caring and skilled urologists to help diagnose, treat and manage your urological problem. If you are experiencing any symptoms of a urological disorder, just visit the institute and have your problem fixed. For more information, visit the “Advanced Urology Institute’” site.
Treatment Options for Urge Incontinence
Urge incontinence is not an inescapable consequence of aging. In fact, a huge majority of women with the condition have been effectively treated or helped. The trick is simply not staying at home and giving up, but visiting a urologist as soon as possible for help.
Factors that affect the treatment decision
Effective treatment of urge incontinence in women depends on the kind of incontinence, personal preferences, underlying causes and severity of the symptoms. Where the condition has more than one underlying cause, the most serious cause will be dealt with first. Likewise, your urologist most likely will opt for the least invasive treatments first before moving on to invasive ones.
Treatments for urge incontinence include:
1. Behavioral techniques
These treatments include making certain lifestyle changes to improve bladder control. They include:
- (a) Bladder training: Entails delaying urination once the urge to pass urine comes. You can begin by holding off urine for as short as 10 minutes and then extending the holding time to hours. The goal of holding off urine each time the urge comes is to lengthen the duration between your trips to the toilet by up to 2.5 hours to 3.5 hours.
- (b) Double voiding: Means that you urinate and then wait for only a short duration (a few minutes) then try again to pass urine. The goal of double voiding is to achieve complete emptying of the bladder to avoid overflow incontinence.
- (c ) Scheduled toilet visits: Planning your toilet trips so that you urinate every 2-4 hours instead of waiting for the urge to come, will help you improve bladder control.
- (d) Diet and fluid management: To improve your bladder control, you may have to cut back or avoid acidic foods, alcohol and caffeinated drinks. By increasing physical activity, reducing liquid consumption or losing weight you can ease urge
incontinence.
2. Pelvic floor exercises
Also called Kegel exercises, pelvic floor exercises can strengthen the muscles responsible for bladder control and urination. To help you learn and perform these exercises, your doctor may recommend that you work with a physical therapist or to try using biofeedback techniques.
3. Electrical stimulation
The urologist may choose to insert electrodes into the vagina to strengthen and stimulate your pelvic floor muscles. With gentle stimulation, urge incontinence may resolve. However, you may need several treatments over many months to be successfully treated.
4. Medications
There are several common medications that are effective in treating urge incontinence. They include:
- (a) Anticholinergics: Include solifenacin (Vesicare), trospium (Sanctura), tolterodine (Detrol), fesoterodine (Toviaz), oxybutynin (Ditropan XL) and darifenacin (Enablex).
- (b) Alpha blockers: These drugs relax bladder muscles and make bladder emptying easier. They include alfuzosin (Uroxatral), doxazosin (Cardura), silodosin (Rapaflo) and tamsulosin (Flomax).
- (c) Topical estrogen: Application of a low dose of a topical estrogen, such as a vaginal patch, cream or ring can rejuvenate and tone the tissues of the vagina and urethra, helping treat urge incontinence.
- (d) Mirabegron (Myrbetriq): This drug relaxes the muscles of the bladder, increases the quantity of urine that the bladder can hold and increases the amount of urine that can be passed at any one time. As a result, it helps to empty the bladder more completely and treats urge incontinence.
5. Medical devices and interventions
Devices such as urethral inserts and pessaries can help to treat or relieve urge incontinence. Interventional therapies such as using a sacral nerve stimulator,bulking material injections, botulinum toxin (Botox) injections and nerve stimulators also can be used to treat urge incontinence.
6. Surgery
The doctor or urologist also may use surgery to correct the underlying cause of urge incontinence. Common surgical procedures include bladder neck suspension, prolapse surgery, artificial urinary sphincter and the sling surgery procedure.
7. Catheters and absorbent pads
If the urologist finds that no medical treatment can completely eliminate the incontinence, various products can be recommended to help ease the problem, minimize discomfort and reduce the inconvenience caused by urine leakage. The most commonly used products are catheters, absorbent pads and absorbent garments.
Urge incontinence is a treatable condition. As a woman, you should not continue living with this problem since there are solutions to help you. At Advanced Urology Institute,we have helped thousands of women with urge incontinence recover from it. Come see us so we can fix the problem. For more information,
visit the “Advanced Urology Institute” site.