Explore the journey of becoming a physician assistant and enhancing patient care here at our office in Orange City, FL.
Continue readingBecoming a Specialist in the Field of Urology
Discover expert care with a specialist in the field of urology. Our dedicated team in Orange City and Daytona Beach, FL are here to help.
Continue readingQuynh Dao Tonnu, PA-C: Removal Procedures for Kidney Stones
Discover effective removal procedures for kidney stones from Quynh Dao-Tonnu, a physician assistant in Orange City, FL.
Continue readingHow Does Stone Location Influence Kidney Stone Treatment Options? – Dr. Arash Rafiei
Dr. Arash Rafiei, a urologist in Orange City, FL addresses how does stone location influence kidney stone treatment options.
Continue readingUnderstanding and Treating Female Incontinence: What Can Advanced Urology Institute Offer?
“Treating female incontinence is taken very seriously once it becomes bothersome” says Dr. Arash Rafiei, a urologist in Orange City, FL.
Continue readingUnderstanding Advanced Prostate Cancer with Chelsie Ferrell, PA
Chelsie Ferrell, physician assistant in Orange City, FL talks about the importance of understanding advanced prostate cancer.
Continue readingChelsie Ferrell, PA: The Pain and Risks of Kidney Stones
Expert Insights: Chelsie Ferrell, PA, on the Pain and Risks of Kidney Stones. Learn How to Prevent & Treat this Common Condition. Read More!
Continue readingHow Has Advanced Urology Institute Revolutionized Urological Care?
Transforming Urological Care: Discover How Advanced Urology Institute Leads the Revolution! Innovations & Patient-Centered Excellence
Continue readingWhy Urology with Dr. Arash Rafiei
Arash Rafiei, a board-certified urologist, discusses the diverse nature of his profession and the importance of staying current with technology advancements. He emphasizes that urology involves a mix of both surgery and medicine.
Continue readingAre You at Risk for Bladder Cancer?
Becoming a Urologist – Dr. Arash Rafiei
Requirements To Become a Urologist
Like Dr. Arash Rafiei, all urologists are required to complete at least three years of college before they enter medical school. Most students complete four years of college with a Bachelor of Science in Chemistry or Biology. After graduation from medical school, the urologist-in-training will complete a residency at a hospital, usually one with a specialty in urology. The residency is a minimum of five years. Time during residency may be split in some programs as two years in general surgery residency and three years in urology. Board certification takes another two to five years. So, effectively, urologists can expect to spend 13 years in study or residency before board certification.
Selecting Your Urologist
 When choosing a urologist, you can specify that you would like a board certified doctor for your urology treatment. Make sure you write down all your questions for the doctor, and seek someone who will take into consideration your individual preferences. Ascertain that the facility and medical staff keep up to date on the latest technologies, such as minimally invasive techniques, as well as proven treatment guidelines.
When choosing a urologist, you can specify that you would like a board certified doctor for your urology treatment. Make sure you write down all your questions for the doctor, and seek someone who will take into consideration your individual preferences. Ascertain that the facility and medical staff keep up to date on the latest technologies, such as minimally invasive techniques, as well as proven treatment guidelines.
What does a Urologist do?
Urologists are medical doctors who specialize in the male and female genitourinary tract, including the urinary bladder, urethra, kidneys, adrenal glands and male reproductive organs. They often diagnose and treat male fertility, prostate cancer, and receive ongoing training in other medical and surgical problems related to these organs.
Advanced Urology Institute is a center for excellence in urology with board-certified specialists to treat all areas of this field. If you need an appointment with a urologist in Orange City, Florida, our team specializes in:
- prostate cancer treatment
- kidney stones
- problems with the bladder, including overactive bladder
- prostatitis
- erectile dysfunction (ED)
- urinary tract infections
- general urology
- and other urology conditions.
Dr. Arash Rafiei, MD is board certified and a member of the American Urological Association, the American College of Surgeons, and the Iranian American Medical Association. For more information, call the office of Dr. Rafiei at (386) 774-2121 or call one of our many Advanced Urology Institute locations. Our doctors will answer your questions and deliver the best service and care based on your needs.
Diagnosing Prostate Cancer
Prostate cancer is the most frequently diagnosed cancer for men, with nearly 10 percent of all men getting it in their senior years. About 99 percent of all prostate cancers occur in men over 50 years old, though younger men should not ignore its risk. While it is one of the most common cancers for men, it also has some of the best survival chances, with over 98 percent of all men diagnosed with prostate cancer surviving at least another five years. This is in part because most prostate cancers grow slowly, and also because there are a lot of simple techniques to notice and diagnose its presence. After diagnosis, there are many effective treatments; however, nearly one out of every 41 men will die from prostate cancer.
Just as women should regularly check their breasts for lumps, men also should check their groin areas. However, that is not commonly taught by most doctors to their male patients, so men should ask their doctors how to do self-examinations.
Other signs that men can check could include any one or more of the following:
- The need to urinate more frequently
- Difficulty in starting to urinate
- Having a weak urine flow (it seems to come out too slow)
- Needing to sometimes rush to the toilet
- Straining to urinate, feeling one’s bladder has not really emptied
- Blood in either your urine or semen (which means something serious!)
 A patient with any one of these symptoms should discuss them with his doctor. If a man has more than one of the symptoms for a week or more, he should see a doctor as soon as possible to check on possible causes. There are also more potentially treatable physical problems not related to the prostate gland that might cause those problems. A general practitioner through some simple tests should be able to then know if a urologist would be required.
A patient with any one of these symptoms should discuss them with his doctor. If a man has more than one of the symptoms for a week or more, he should see a doctor as soon as possible to check on possible causes. There are also more potentially treatable physical problems not related to the prostate gland that might cause those problems. A general practitioner through some simple tests should be able to then know if a urologist would be required.
Those uncomfortable “digital” rectal exams (DRE) men are asked to undergo can also detect prostate cancer, as well as another non-cancerous condition that can cause an enlarged prostate (BPH). If a general practitioner detects something unusual from a DRE that seems to be prostate-related, a prostate-specific antigen (PSA) blood test usually will be ordered. PSA is a prostrate-made substance that will tend to increase when men have cancer, inflammation, or even a simple infection of the prostate gland. Medical specialists will know when the PSA counts require specialists like those at the Advanced Urology Institute to further examine the patient.
A urology clinic can do most, if not all the following tests to determine if prostate cancer is the problem. They can use a transrectal ultrasound to get an ultrasound picture of the prostate gland and surrounding tissues. X-rays can detect if a cancer has potentially spread in a visible way. If the urologists determine there clearly are issues with the prostate, they perform a biopsy to discover the grade of the cancer, to discover how potentially aggressive the cancer is. A transrectal magnetic resonance imaging (MRI) may be required since some types of prostate cancer can spread out of the prostate into surrounding tissues and bones. Bone scans also may be utilized. Genetic tests on the biopsied tissues will help determine how aggressive the cancer may be. The clinic may use other types of exams and tests, depending upon medical findings.
After the urologist has completed the medical evaluations, the chances of recovery, the prognosis, can be discussed with the patient as well as the treatment options. The board-certified specialists at various clinics of the Advanced Urology Institute have years of experience working with patients, giving them the best advice for each of their unique situations. For more information, visit the Advanced Urology Institute website.
What is MRI with Transrectal Ultrasound Fusion-Guided Prostate Biopsy
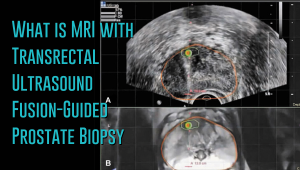 Prostate cancer has a new standard of care in MRI-guided fusion biopsy with transrectal ultrasound. While a prostate biopsy has been the only way to get a definitive diagnosis of prostate cancer, it has only been working if cancer cells are identified in the sample tissue. But in some cases, such as when the tumor occurs at the top surface of the prostate or other unusual locations, a biopsy may not give a correct diagnosis. For instance, the standard TRUS (transrectal ultrasound) guided biopsy in which tissue samples are collected from the prostate in a systematic pattern gives a negative result with tumors located in unusual areas of the prostate. About 15-20 percent of tumor locations can be missed by the biopsy needle.
Prostate cancer has a new standard of care in MRI-guided fusion biopsy with transrectal ultrasound. While a prostate biopsy has been the only way to get a definitive diagnosis of prostate cancer, it has only been working if cancer cells are identified in the sample tissue. But in some cases, such as when the tumor occurs at the top surface of the prostate or other unusual locations, a biopsy may not give a correct diagnosis. For instance, the standard TRUS (transrectal ultrasound) guided biopsy in which tissue samples are collected from the prostate in a systematic pattern gives a negative result with tumors located in unusual areas of the prostate. About 15-20 percent of tumor locations can be missed by the biopsy needle.
What makes the MRI-ultrasound fusion biopsy more definitive?
The MRI-ultrasound fusion approach is an improvement on the traditional 12-core TRUS, which involved taking biopsies from twelve prostate areas where the cancer is considered more likely to occur. With the TRUS biopsy, about 70 percent of men who have a negative biopsy result are not essentially free of the cancer. The MRI-ultrasound fusion technology blends the superior imaging capability of the high-definition multi-parametric (mp) MRI with real-time ultrasound imaging. There is better visualization of the suspicious areas of the prostate where the cancer may occur that may not be visible on ultrasound alone. The fusion-guided biopsy detects almost twice as many prostate cancers in all stages as the standard TRUS biopsy.
The ability of MRI-ultrasound fusion-guided biopsy to create a three-dimensional (3D) map of the prostate ensures that doctors are able to see the targeted areas of the prostate better and perform more precise biopsies. The technology uses a machine known as UroNav developed by Invivo, which is supplied with sophisticated software to produce super-detailed MRI images and fuse them with the ultrasound images generated by a transrectal probe administered on the patient in an outpatient setting. The resulting images enable the examining physician to direct biopsy needles with pinpoint accuracy and to easily access any lesions or suspicious areas revealed by MRI. The technology allows the urologist to hit the target spot more accurately and improves cancer detection rate. In fact, it is primarily used for men who have an ongoing suspicion of prostate cancer, such as those with consistently elevated PSA, but whose TRUS biopsy results are repeatedly negative.
Fewer biopsies, more accurate detection
The fusion-guided biopsy is a very targeted approach in which biopsies are performed only in highly suspicious areas of the prostate appearing in the MRI image. As a result, significantly fewer biopsies are done with the MRI-ultrasound fusion than with the traditional TRUS technique, minimizing the adverse effects that often accompany repeat biopsies. Multiple prostate biopsies can lead to complications such as bleeding, infection, urinary retention problems, sepsis or even death.
In spite of fewer biopsies, the MRI fusion approach increases the rate of detection of aggressive prostate cancer. The extensive MRI images obtained before the biopsy helps highlight both high-risk and intermediate-risk cancers often missed by traditional TRUS biopsy. With MRI-ultrasound fusion, the likelihood of detecting cancer increases as the grade of the tumor increases. The use of MRI fusion biopsy helps to avoid metastatic disease by finding cancer before it spreads to other areas of the body.
Improved cancer differentiation
Through MRI fusion, doctors are able to more accurately differentiate cancers that require treatment from the ones that should undergo watchful waiting (active surveillance). Fusion technology is able to show higher-risk cancers and does not highlight the insignificant low-grade tumors, making it less likely for urologic oncologists to over-treat indolent and low-grade cancers. A number of prostate cancers are low-grade, non-aggressive and do not cause problems at all and treating them through chemotherapy, radiotherapy or surgery can impair the quality of life or even cause death. MRI fusion effectively saves patients from the adverse effects of treating low-grade tumors. Fusion technology eliminates up to 50 percent of prostate cancer treatments that are unnecessarily administered on low-grade cancers.
At Advanced Urology Institute, we have adopted the MRI-ultrasound fusion biopsy and changed the way we screen, evaluate and diagnose prostate cancer. It has become our standard for detecting prostate cancer and we believe in the next few years it will be the gold standard for detecting the cancer. We are proud that it offers a higher detection rate, superior accuracy and reduces the rate of repeat biopsies — making our practice one of the best places for detection and monitoring of the cancer. It helps us deliver the best treatment outcomes for our patients.
If you think you are at high risk of prostate cancer or already have started experiencing some symptoms, let us show you how the precision of our high-definition MRI fusion machine, the expertise of our skilled physicians in MRI fusion biopsy and the know-how of our radiologists proficient in multi-parametric MRI imaging can help you. For more information on the treatment and diagnosis of prostate cancer, visit the “Advanced Urology Institute” site.
Why I Love Urology! Treating and Curing Urological Conditions
Why I Love Urology! Treating and Curing Urological Conditions
Urologists love their jobs because it gives them opportunities to provide patients with life saving treatments as well as quality of life medical care. Conditions such as cancer of the testes, if diagnosed early, can be treated to give the patient a longer life span and one free of discomfort or pain during intimacy.
It is important to note that the work of a urologist also involves educating the general public on effective prevention practices. A good example is prostate cancer, an illness which has been on the rise recently. Research has identified potential causes, prevention and treatment. This knowledge has been shared widely by urologists. Men are now encouraged to use testing for early diagnosis. If caught in the primary stages, prostate cancer can be cured before it progresses to stage IV cancer or metastasizes to other parts of the body. The same applies to other conditions such as erectile dysfunction, a topic most men prefer to avoid. Despite the reluctance to acknowledge this medical problem, in recent years the public has been receiving education from the experts on the many causes and treatments of erectile dysfunction.
Urology is a field that specializes in treating urological physical ailments and the emotional concerns that accompany them. Each patient presents with different needs and urologists who love the work they do understand that. They take into account the presenting factors of each patient, their needs and concerns, and then tailor the consultations, medical treatment and follow up to suit the unique needs of each patient. Any person with concerns about a potential urological problem should pay a visit to a qualified specialist for a check-up. The experienced and caring professionals of the Advanced Urology Institute would like to remind us that the earlier a problem is diagnosed, the more successful the treatment will be.
What I Do as a Physician Assistant – Lisa Cunningham
What I Do as a Physician Assistant – Lisa Cunningham
Physician assistants act as the liaison between the competing demands of patients, staff and family on their attending physician’s time. [Read Full Article…]