AUI’s Windsor Oaks Office is proud to feature a remarkable group of urologists and providers with a passion for patient care.
Continue readingExperience Premier Urology Care at Timber Ridge Office
What is MRI with Transrectal Ultrasound Fusion-Guided Prostate Biopsy
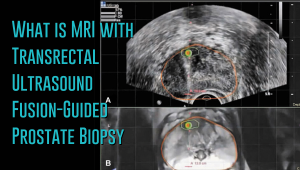 Prostate cancer has a new standard of care in MRI-guided fusion biopsy with transrectal ultrasound. While a prostate biopsy has been the only way to get a definitive diagnosis of prostate cancer, it has only been working if cancer cells are identified in the sample tissue. But in some cases, such as when the tumor occurs at the top surface of the prostate or other unusual locations, a biopsy may not give a correct diagnosis. For instance, the standard TRUS (transrectal ultrasound) guided biopsy in which tissue samples are collected from the prostate in a systematic pattern gives a negative result with tumors located in unusual areas of the prostate. About 15-20 percent of tumor locations can be missed by the biopsy needle.
Prostate cancer has a new standard of care in MRI-guided fusion biopsy with transrectal ultrasound. While a prostate biopsy has been the only way to get a definitive diagnosis of prostate cancer, it has only been working if cancer cells are identified in the sample tissue. But in some cases, such as when the tumor occurs at the top surface of the prostate or other unusual locations, a biopsy may not give a correct diagnosis. For instance, the standard TRUS (transrectal ultrasound) guided biopsy in which tissue samples are collected from the prostate in a systematic pattern gives a negative result with tumors located in unusual areas of the prostate. About 15-20 percent of tumor locations can be missed by the biopsy needle.
What makes the MRI-ultrasound fusion biopsy more definitive?
The MRI-ultrasound fusion approach is an improvement on the traditional 12-core TRUS, which involved taking biopsies from twelve prostate areas where the cancer is considered more likely to occur. With the TRUS biopsy, about 70 percent of men who have a negative biopsy result are not essentially free of the cancer. The MRI-ultrasound fusion technology blends the superior imaging capability of the high-definition multi-parametric (mp) MRI with real-time ultrasound imaging. There is better visualization of the suspicious areas of the prostate where the cancer may occur that may not be visible on ultrasound alone. The fusion-guided biopsy detects almost twice as many prostate cancers in all stages as the standard TRUS biopsy.
The ability of MRI-ultrasound fusion-guided biopsy to create a three-dimensional (3D) map of the prostate ensures that doctors are able to see the targeted areas of the prostate better and perform more precise biopsies. The technology uses a machine known as UroNav developed by Invivo, which is supplied with sophisticated software to produce super-detailed MRI images and fuse them with the ultrasound images generated by a transrectal probe administered on the patient in an outpatient setting. The resulting images enable the examining physician to direct biopsy needles with pinpoint accuracy and to easily access any lesions or suspicious areas revealed by MRI. The technology allows the urologist to hit the target spot more accurately and improves cancer detection rate. In fact, it is primarily used for men who have an ongoing suspicion of prostate cancer, such as those with consistently elevated PSA, but whose TRUS biopsy results are repeatedly negative.
Fewer biopsies, more accurate detection
The fusion-guided biopsy is a very targeted approach in which biopsies are performed only in highly suspicious areas of the prostate appearing in the MRI image. As a result, significantly fewer biopsies are done with the MRI-ultrasound fusion than with the traditional TRUS technique, minimizing the adverse effects that often accompany repeat biopsies. Multiple prostate biopsies can lead to complications such as bleeding, infection, urinary retention problems, sepsis or even death.
In spite of fewer biopsies, the MRI fusion approach increases the rate of detection of aggressive prostate cancer. The extensive MRI images obtained before the biopsy helps highlight both high-risk and intermediate-risk cancers often missed by traditional TRUS biopsy. With MRI-ultrasound fusion, the likelihood of detecting cancer increases as the grade of the tumor increases. The use of MRI fusion biopsy helps to avoid metastatic disease by finding cancer before it spreads to other areas of the body.
Improved cancer differentiation
Through MRI fusion, doctors are able to more accurately differentiate cancers that require treatment from the ones that should undergo watchful waiting (active surveillance). Fusion technology is able to show higher-risk cancers and does not highlight the insignificant low-grade tumors, making it less likely for urologic oncologists to over-treat indolent and low-grade cancers. A number of prostate cancers are low-grade, non-aggressive and do not cause problems at all and treating them through chemotherapy, radiotherapy or surgery can impair the quality of life or even cause death. MRI fusion effectively saves patients from the adverse effects of treating low-grade tumors. Fusion technology eliminates up to 50 percent of prostate cancer treatments that are unnecessarily administered on low-grade cancers.
At Advanced Urology Institute, we have adopted the MRI-ultrasound fusion biopsy and changed the way we screen, evaluate and diagnose prostate cancer. It has become our standard for detecting prostate cancer and we believe in the next few years it will be the gold standard for detecting the cancer. We are proud that it offers a higher detection rate, superior accuracy and reduces the rate of repeat biopsies — making our practice one of the best places for detection and monitoring of the cancer. It helps us deliver the best treatment outcomes for our patients.
If you think you are at high risk of prostate cancer or already have started experiencing some symptoms, let us show you how the precision of our high-definition MRI fusion machine, the expertise of our skilled physicians in MRI fusion biopsy and the know-how of our radiologists proficient in multi-parametric MRI imaging can help you. For more information on the treatment and diagnosis of prostate cancer, visit the “Advanced Urology Institute” site.
Professionalism and Personalized Care in a Doctor-Patient Relationship
Video: Professionalism and Personalized Care in a Doctor-Patient Relationship
The doctor-patient relationship is the foundation of all good healthcare. Delivering quality care depends, to a great extent, on the quality of communication. [Read Full Article…]
How Are Genetics Transforming Our World? Dr. Saumil Karavadia Explores the Latest Advancements
The Prostate Gland
Video: Testosterone Therapy – Diagnosing Low Testosterone Levels
For some men, difficulty urinating is often a sign of either an enlarged prostate or an inflammation of the prostate, called prostatitis. Early prostate cancer does not usually cause problems with urination. [Read Full Article…]
How Does the da Vinci Robotics System Revolutionize Surgery Explained by Dr. Karavadia
Do You Need Testosterone Therapy? Learn How Urologists Like Dr. Edward King Treat Low Testosterone
Is Testosterone Therapy Right for You? Dr. Karavadia Explains How to Diagnose Low Levels
What’s the Debate About PSA Testing? Dr. Edward King Clarifies the Controversial PSA Test
Prostate Cancer – Risk Factors and Screening
Video: Prostate Cancer – Risk Factors and Screening
One of the major characteristics of prostate cancer is that it grows very slowly. The cancerous cells in the prostate can remain without symptoms for decades. This is why almost 75% of men with prostate cancer never even know they have a cancerous growth. Contact a urologist now and get treatment for this condition as soon as possible. [Read Full Article…]
What Can You Expect During Prostate Cancer Recovery? Insights from Dr. Saumil Karavadia
An Individual Approach to Treating Prostate Cancer
Video: An Individual Approach to Treating Prostate Cancer
After confirming a prostate cancer diagnosis, physicians proceed to determining the aggressiveness of the disease. This is called “cancer grading.” The pathologist will use the biopsy preparations to assess the differences between normal cancer cells and cancerous prostate cells. [Read Full Article…]
Prostate Cancer – Understanding Your Options
Video: Prostate Cancer – Understanding Your Options
There are many treatment options for prostate cancer. Depending upon the stage of the disease, robotic surgery, radiation therapy, cryoablation, hormonal therapy and even watchful waiting are some of the alternatives to be considered. Contact a urologist now and get treatment for this condition as soon as possible. [Read Full Article…]
Kidney Stones – Environmental Factors Can Increase the Risk
Video: Urology is The Perfect Specialty for Me by Dr Thomas Sander
A kidney stone is a mass of chemical crystals that forms in the kidney, ureter or bladder of an individual. Such stones may develop to different sizes and in different shapes, from tiny microscopic crystals to quite large stones. Kidney stones can occur at any age but are far more prevalent between the ages of 20 to 40. Contact a urologist now and get treatment for this condition as soon as possible. [Read Full Article…]





