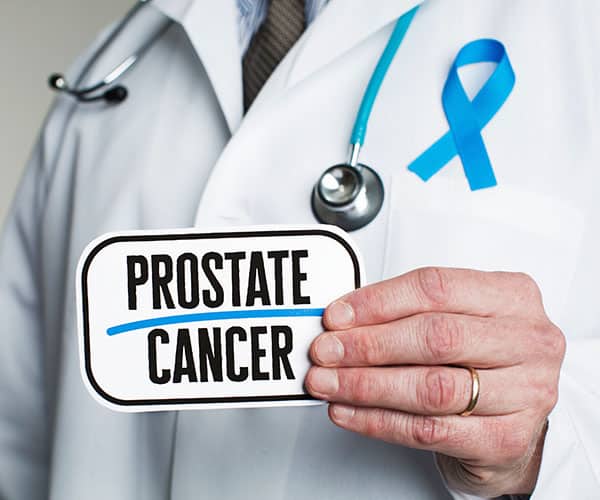
Most Floridians know how to make a “go” bag in case of a hurricane. But what’s in your “go” bag in the case of prostate cancer?
In Florida, 113 of every 100,000 men are diagnosed with prostate cancer. It is the second most common cancer in men following skin cancer – a condition for which Floridians know how to prepare.
Sure, few men want to get ready for any cancer, including that of the prostate. But if you are among those men recently diagnosed, there are steps you can take to better adapt to your treatment and recovery.
Here’s what you can expect, and why.
Why Prostate Cancer Can Be Cured
Your prostate is a 1-ounce gland that helps make the fluid that carries semen. It’s located in an active part of your body, beneath your bladder and around the urethra.
Cancer occurs when an abnormality makes the cells grow out of control, without stopping, until they form a tumor. When this happens in the prostate, the cancer tends to grow slowly, so it is usually caught before spreading to surrounding tissue and bones.
Symptoms include difficulty urinating, blood in your urine or semen, unexplained weight loss, and pain in the groin area. If the cancer has spread, your bones might hurt.
Your chances of developing prostate cancer can vary based on age, race, family history, and lifestyle, but overall prevalence has risen 3% a year since 2014. The good news is that 99% of men diagnosed with localized prostate cancer today survive.
Choosing the Right Treatment for You
If you are diagnosed with prostate cancer, you’ll have a choice of treatments based on the stage and aggressiveness of the disease. In 40% of localized cases, men have their prostates surgically removed (prostatectomy). Other options include radiation therapy and, if the cancer is low risk, surveillance with repeat testing.
In cases where the cancer has spread beyond the prostate, your doctor could advise immunotherapy, chemotherapy, radiation, or hormone therapy to block testosterone production and slow the cancer.
Life After Prostate Cancer: Changes to Expect
During and after your treatment, you will experience some differences in your body and lifestyle. Following are the most common.
Scheduled time off of work – Men who have prostate surgery should plan to take three to four weeks off from work, depending on job physicality. If you work from home, you could return sooner.
Bathroom issues – A prostatectomy requires removal of one of the urinary valves (sphincters), resulting in incontinence in 6% to 8% of patients. This typically lasts a few months to a year. In some men, radiation therapy weakens the bladder. Kegel exercises can help.
Reduced drive in bed – Some procedures could affect the nerves and blood vessels that help you get an erection, but this could be treatable. Hormone therapy might temporarily weaken your sex drive. If the prostate is removed, you can still achieve orgasm, but will not ejaculate.
Limited activity and fats – You’ll have to take it easy after surgery – no strenuous exercise and heavy lifting for a month. You should be able to do Kegels and low-impact activities. And what you eat matters more: reduce fatty foods and red meat in favor of fruits and vegetables.
Therapy side effects – If you undergo chemotherapy, you might experience nausea, hair loss, and fatigue. Side effects of hormone treatments include thinning bones, hot flashes, and weight gain.
Get Your Prostate Cancer “Go” Bag Ready
Above all, your life after prostate cancer will require steps to remain cancer free. Expect to see your doctor every few months for a prostate exam and prostate-specific antigen (PSA) test, which detects cell abnormalities.
The better prepared you are now, physically and emotionally, the sooner you can enjoy the calm after the storm.
You can read more about our prostate cancer diagnostics and treatments on our website. Learn about clinical trials at AUI.











 As men age, their prostate grows and they’re more likely to experience benign prostatic hyperplasia (BPH) – or an
As men age, their prostate grows and they’re more likely to experience benign prostatic hyperplasia (BPH) – or an