KEY TAKEAWAYS:
- The Advanced Urology Institute’s Naples office, led by Dr. Rolando Rivera, offers a range of outpatient urology procedures, including prostate procedures, reconstructive surgeries, and stone disease treatment.
- Complex cases requiring specialized equipment, such as robotic surgery for pelvic organ prolapse, are performed at the hospital.
- The Advanced Urology Institute is the largest urology practice in Florida, providing comprehensive and personalized care to patients seeking a urologist in Naples, FL.
Introduction
Urology is a specialized field of medicine that focuses on the diagnosis, treatment, and management of various conditions related to the urinary tract and male reproductive system. At the Advanced Urology Institute in Naples, Florida, Dr. Rolando Rivera, is a board-certified urologist who is also specialized in Female Pelvic Medicine and Reconstructive Surgery. In this article, we will discuss the various urology procedures performed at the Naples office and how Dr. Rivera can help you.
Outpatient Urology Procedures in Naples
The surgery center in Naples is designed for primarily outpatient interventions that are fairly uncomplicated. A range of procedures can be performed at this facility, catering to the diverse needs of patients seeking a urologist in Naples, FL.
Prostate Procedures
One of the common procedures performed at the Naples office is the Urolift. This minimally invasive procedure treats benign prostatic hyperplasia (BPH), a condition characterized by an enlarged prostate gland. The Urolift procedure involves the placement of small implants to lift and hold the enlarged prostate tissue out of the way, relieving pressure on the urethra and improving urine flow.
Reconstructive Surgeries
Dr. Rolando Rivera performs simple reconstructive procedures at the Naples office, focusing on pelvic reconstructive surgeries. These surgeries address issues such as pelvic organ prolapse, in which the pelvic organs, like the bladder or uterus, descend due to weakened pelvic floor muscles and ligaments. The reconstructive procedures aim to repair and strengthen the pelvic floor to restore normal function and alleviate symptoms.
Stone Disease Treatment
For patients suffering from kidney stones, the Naples office offers various treatment options. Depending on the size, location, and type of kidney stones, Dr. Rivera may perform minimally invasive procedures like extracorporeal shock wave lithotripsy (ESWL) or ureteroscopy to break up and remove the stones.
Hospital Procedures for Complex Cases
While the Naples office is equipped to handle a variety of urological issues, some complex cases require specialized equipment and hospital facilities. For instance, Dr. Rivera performs robotic surgery for pelvic organ prolapse at the hospital. This advanced technique uses the da Vinci Surgical System to perform precise, minimally invasive procedures that result in shorter recovery times and reduced complications.
Advanced Urology Institute: Comprehensive Urological Care
The Advanced Urology Institute is the largest urology practice in Florida, offering state-of-the-art facilities and a team of highly skilled urologists. With a focus on providing personalized care to each patient, the team at the Advanced Urology Institute works collaboratively to diagnose and treat a wide range of urological conditions. If you are seeking a urologist in Naples, FL, trust the expertise of Dr. Rolando Rivera and the team at the Advanced Urology Institute.
TRANSCRIPTION:
I’m Rolando Rivera and I’m board certified in Urology and Female Public Medicine and Reconstructed Surgery with Advanced Urology Institute.
So the surgery center is designed for primary outpatient interventions that are fairly uncomplicated. So we do do a fair amount of things in the surgery center. We do our prostate procedures, Urolift, we do a fair amount of those. We do simple reconstructive procedures, public reconstructive surgeries, stone disease, those kinds of things. The more complex reconstructive surgeries that require specific equipment, like I do robotic surgery for prolapse, that is a hospital procedure.
REFERENCES:
- “Female Pelvic Medicine and Reconstructive Surgery | Cedars-Sinai.” https://www.cedars-sinai.org/programs/urology-academic-practice/clinical/female.html.
- “UroLift for Benign Prostatic Hyperplasia (BPH) – UCLA Health.” https://www.uclahealth.org/medical-services/urology/conditions-treated/male-conditions/urolift-benign-prostatic-hyperplasia-bph.
- “Extracorporeal Shock Wave Lithotripsy (ESWL).” https://www.hopkinsmedicine.org/health/conditions-and-diseases/kidney-stones/extracorporeal-shock-wave-lithotripsy-eswl.




 The different
The different 
 Fortunately for men who suffer from BPH, medical progress is on their side. According to
Fortunately for men who suffer from BPH, medical progress is on their side. According to 
 Once an appointment is made with the urologist, doctor and patient can begin discussing symptoms and the diagnostic process. If the patient’s complaints are consistent with BPH, the urologist will proceed with a prostate exam. There are also other simple, non-invasive tests that can be completed at the urologist’s office that will indicate the patient’s urine flow and ability to empty his bladder. More sophisticated testing is available if additional data on the patient’s BPH issue is needed. For example, fiber optic scope evaluations give the urologist the most detailed picture of the patient’s BPH, which can then be used to devise the best treatment plan.
Once an appointment is made with the urologist, doctor and patient can begin discussing symptoms and the diagnostic process. If the patient’s complaints are consistent with BPH, the urologist will proceed with a prostate exam. There are also other simple, non-invasive tests that can be completed at the urologist’s office that will indicate the patient’s urine flow and ability to empty his bladder. More sophisticated testing is available if additional data on the patient’s BPH issue is needed. For example, fiber optic scope evaluations give the urologist the most detailed picture of the patient’s BPH, which can then be used to devise the best treatment plan.
 (UTIs) are another issue that brings many women, especially older women, to their urologist’s office. UTIs are another urinary issue that can affect both men and women, but they are far more common in women than men. About half of all women will have a UTI in their lifetimes, while only 1 in 10 men will. UTIs are infections that happen in the bladder or urethra. Symptoms include burning while urinating, frequent urges to urinate, and pain in the lower back and abdomen. Urologists can prescribe antibiotics to treat the infection.
(UTIs) are another issue that brings many women, especially older women, to their urologist’s office. UTIs are another urinary issue that can affect both men and women, but they are far more common in women than men. About half of all women will have a UTI in their lifetimes, while only 1 in 10 men will. UTIs are infections that happen in the bladder or urethra. Symptoms include burning while urinating, frequent urges to urinate, and pain in the lower back and abdomen. Urologists can prescribe antibiotics to treat the infection.
 OXFORD, FL, October 30, 2020 — Advanced Urology Institute is proud to announce that Dr. Scott B. Sellinger will become president in 2021.
OXFORD, FL, October 30, 2020 — Advanced Urology Institute is proud to announce that Dr. Scott B. Sellinger will become president in 2021.
 One reason men see a urologist is to check for prostate cancer. Prostate cancer is the most common form of cancer that affects men. As they age and their likelihood of developing the disease increases, regular prostate cancer screenings by a urologist become increasingly important. If cancer is found, the urologist will discuss treatment options with the patient. Some non-aggressive cases can be treated simply by monitoring the cancer. Others cases may need to be treated with surgery or radiation therapy.
One reason men see a urologist is to check for prostate cancer. Prostate cancer is the most common form of cancer that affects men. As they age and their likelihood of developing the disease increases, regular prostate cancer screenings by a urologist become increasingly important. If cancer is found, the urologist will discuss treatment options with the patient. Some non-aggressive cases can be treated simply by monitoring the cancer. Others cases may need to be treated with surgery or radiation therapy.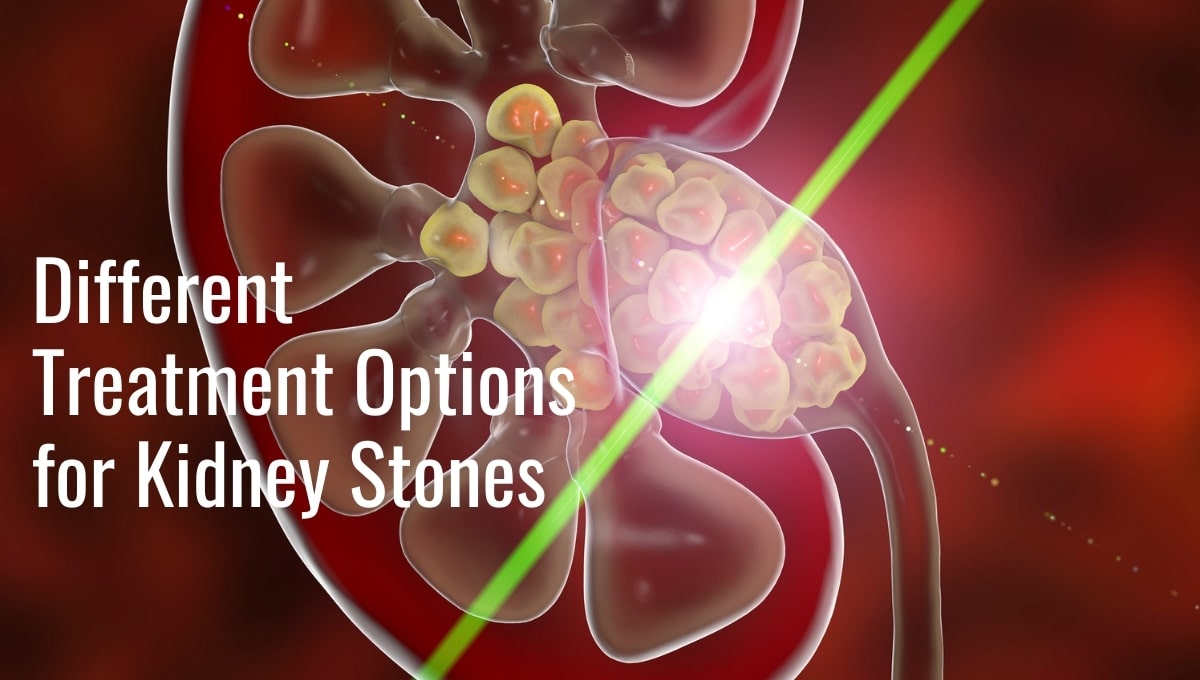

 For many men, their prostate cancer will not be aggressive and the symptoms will be manageable. In these cases, urologists rely on active surveillance as the best first treatment option. Rather than risk possibly harmful treatments on a non-aggressive cancer, the urologist will monitor the cancer with routine checkups. Other treatment options will be considered if the cancer becomes more aggressive.
For many men, their prostate cancer will not be aggressive and the symptoms will be manageable. In these cases, urologists rely on active surveillance as the best first treatment option. Rather than risk possibly harmful treatments on a non-aggressive cancer, the urologist will monitor the cancer with routine checkups. Other treatment options will be considered if the cancer becomes more aggressive.


 One of the biggest benefits of immunotherapy is its less severe side effects.
One of the biggest benefits of immunotherapy is its less severe side effects. 
 These
These 
 This focused biopsy is called a
This focused biopsy is called a