Urology is a fascinating, stimulating and satisfying field of medicine. As urologists, we treat conditions of the urinary tract in both men and women, together with disorders of the male reproductive system. Being a urologist is an opportunity to care for people with agonizing, embarrassing and life-threatening conditions, such as kidney stones, urinary incontinence, erectile dysfunction, and genitourinary cancers, restoring normalcy in their lives. For those like me who are passionate about saving and improving lives, urology is a worthwhile career. For me, every day spent with my patients is not only an opportunity to serve and help people, but also contribute to saving or extending lives. In turn, the positive outcomes from various interventions bring joy and satisfaction.
Why urology?
Well, mine is a funny story. Growing up in Lansing, Mi., with both my parents having PHDs — my mother working at the Lansing School District and my father being a Michigan University professor — I learned to be inquisitive from a very early age. Being educators, my parents always encouraged me to be curious; to try to understand how various things worked. Eventually I became profoundly curious about how my body works and searched for answers wherever I could find them. As a result, I ended up studying physiology, then medicine, and ultimately specializing in urology.
Path to urology
 My curiosity led me to study physiology — the study of how the body works — to learn more about the body. So I attended Michigan State University to pursue a Bachelor of Science degree in physiology. As I was studying physiology, I became interested in medicine. Upon graduation, I went to Ann Arbor, University of Michigan for my medical education. After that, I moved to Henry Ford Hospital for my residency training before going to and completing my fellowship training at the Beth Israel Deaconess Medical Center.
My curiosity led me to study physiology — the study of how the body works — to learn more about the body. So I attended Michigan State University to pursue a Bachelor of Science degree in physiology. As I was studying physiology, I became interested in medicine. Upon graduation, I went to Ann Arbor, University of Michigan for my medical education. After that, I moved to Henry Ford Hospital for my residency training before going to and completing my fellowship training at the Beth Israel Deaconess Medical Center.
During clinical rotations in medical school I came across urology. I actually did not know anything about urology until my classmates at medical school told me about it. They really took me under their wings like a little brother. And because they liked me and I liked them, we were able to speak freely about our career aspirations and interests. So when they recommended that I study urology, telling me repeatedly that I had to try urology —”stay here and be a urologist’ — I gave it a shot and here I am, a board-certified urologist.
What does it take to be a urologist?
As urologists, we see the whole spectrum of age groups — from newborns to elderly patients. For instance, we can see children with congenital problems and care for geriatric patients with bladder control problems, sexual dysfunction or benign prostatic enlargement. So we delve into deeply emotional problems that require empathy, support and effective solutions.
That is why to be a good urologist, you need not only to understand medicine very well and be able to offer effective treatments, but you also must have emotional intelligence. That is, you need to know what to say, why to say it, when to say it and how to say it, and to treat patients as human beings, handling them in a warm, friendly and respectful manner. Actually, honesty, empathy and compassion are the marks of a proficient urologist.
Areas of expertise
I have practiced urology for several years now, seeing patients for a broad range of issues. Frequently I treat patients with enlarged prostate, urinary stones, urinary incontinence, prostatitis, testicular pain, recurrent urinary tract infections, urologic cancers and erectile dysfunction. But my areas of special interest include voiding dysfunction, pelvic floor reconstruction, urinary incontinence, female urology, urodynamics, and urogenital disorders triggered by neurologic disorders.
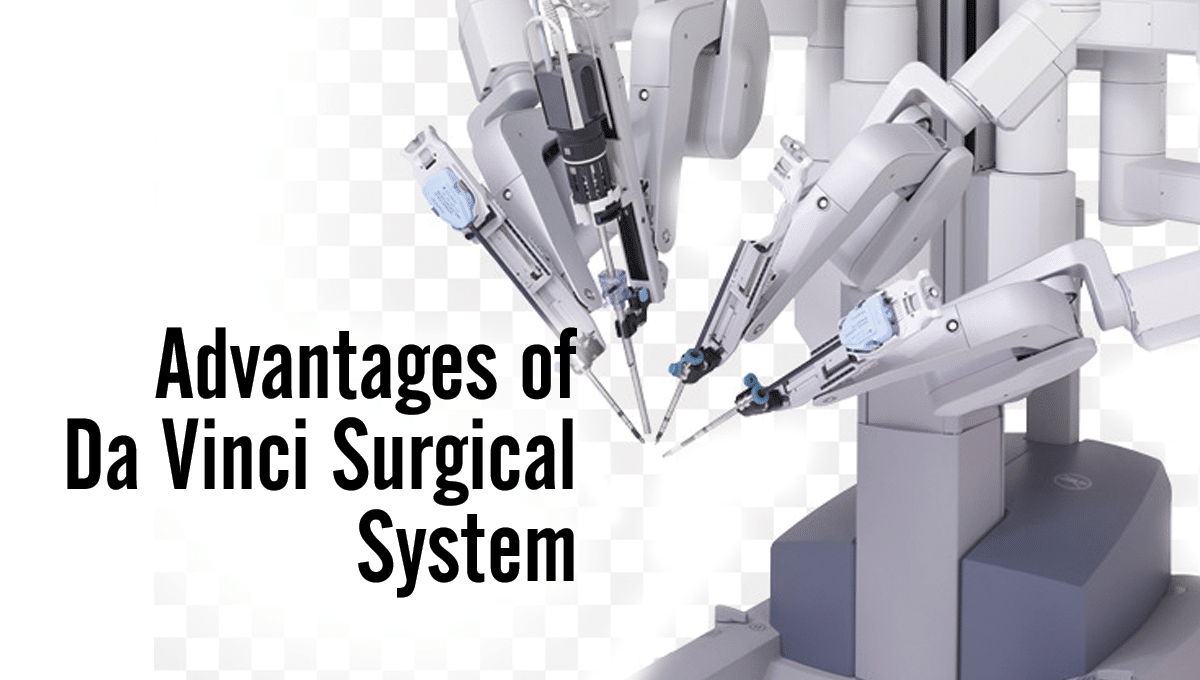
Over the years, I have performed pelvic floor reconstruction surgeries in both men and women, neuromodulation, surgery for bladder dysfunction, MonaLisa Touch laser procedure for post-menopausal sexual and urinary symptoms, Botox (botulinum toxin) injections, UroLift System procedure for BPH, and da Vinci robotic treatment for post-menopausal sexual and urinary symptoms. I also keep improving my knowledge and refining my skills through continuous medical education, training and research. I understand that I can only deliver the best to my patients when I have the right skills, tools and methods.
Job satisfaction
Urology is about providing relief to people with troubling and humiliating conditions. Patients come to us when they are at some of the lowest moments of their lives and we are able to address their issues and see them restored to normal lives again. Something unique about urology is that the problems we handle are often clearly defined, which means that almost every time a patient presents with a urological condition, we are able to pinpoint the exact etiology and extent of defect and then provide an effective solution.
Therefore, we are able to achieve great outcomes for almost all our patients. In fact, unlike other specialties such as neurology and oncology, the majority of our patients get better and do well after interacting with us. And with this understanding that we can solve many — if not most — of the urologic issues of our patients, we really feel satisfied with our work. And since we are able to achieve great results for our patients, they are always grateful and hold us in high esteem. So with urology, we are largely contented and happy about the work we do.
Why Advanced Urology Institute?
Urologists need a working environment that can bring out the best of their knowledge, skills and talents. For me, that dream place is Advanced Urology Institute. At AUI, all administrative tasks are centralized to ensure that physicians find enough time to deliver the best possible care. Urologists also have access to cutting-edge surgical and medical equipment and are able to apply the latest methods and techniques as soon as they are available.
Urologists at AUI work under a thriving culture of compassionate, collaborative and multidisciplinary approach to patient care, which enables frequent cooperation with other board-certified, skilled and experienced medical professionals. To crown it all, AUI clinics are always warm, friendly and buzzing with colleagues sharing stories, cracking jokes and interacting freely. It is always a wonderful experience being at AUI and I really feel privileged being part of the team.
Want to know more about AUI and the services we offer? Find out more by visiting the “Advanced Urology Institute” site.
TRANSCRIPTION:
I’m Jonathan Jay, I’m a board-certified urologist with Advanced Urology Institute.
Funny story, I just had a curiosity about how my body worked, so that led me into physiology because that was a study of how your body really works and then with time that just led into medicine.
Lansing Michigan, my family and my parents were educators, both PhDs, my mother working in Lansing School District, my father worked for Michigan State University as a professor.
Interesting enough, education was important in my family. I always had a curiosity about learning and understanding things, so that’s what they gave me, they gave me a curiosity of trying to understand things.
It’s funny, urology came about by a rotation through medical school, all the medical school students said, hey you got to try urology, they let the medical school, medical students close the wounds, that’s a pretty rare thing.
So all the guys were very nice, these guys took me under their wing like a little brother and so with that they said, hey why don’t you, they liked me, I liked them, they said why don’t you stay here and be a urologist.
Now urology was something that I never even knew existed, in fact they gave a lecture in the second year of medical school, I said who would want to do that, that is the grossest thing I’ve ever seen, but here I am being a urologist all because of a great experience that people provided me, took me under their wing like a little brother. So for me, I always felt like being a doctor you had to have four qualities. The first quality you had to have is you had to understand medicine. You don’t have to be the valedictorian of the class, but you got to understand medicine fairly well.
The next thing you have to have is stellar social intelligence. You got to be able to talk to a human being like a human being, be able to read social cues, know what to say, when to say and how to say it. Then above all you have to care and have empathy for another human being. You have to have all four of those qualities.
REFERENCES:
 Reconstructive surgery is a testimony to how much technology has improved the practice of medicine. In cases of pelvic organ prolapse, the surgery is performed to restore the affected organ to its proper place. There are different types of reconstructive surgery, depending on the type of organ prolapse being treated. Whatever the type of reconstructive surgery, however, it is a minimally invasive procedure.
Reconstructive surgery is a testimony to how much technology has improved the practice of medicine. In cases of pelvic organ prolapse, the surgery is performed to restore the affected organ to its proper place. There are different types of reconstructive surgery, depending on the type of organ prolapse being treated. Whatever the type of reconstructive surgery, however, it is a minimally invasive procedure.







 My curiosity led me to study physiology — the study of how the body works — to learn more about the body. So I attended Michigan State University to pursue a Bachelor of Science degree in physiology. As I was studying physiology, I became interested in medicine. Upon graduation, I went to Ann Arbor, University of Michigan for my medical education. After that, I moved to Henry Ford Hospital for my residency training before going to and completing my fellowship training at the Beth Israel Deaconess Medical Center.
My curiosity led me to study physiology — the study of how the body works — to learn more about the body. So I attended Michigan State University to pursue a Bachelor of Science degree in physiology. As I was studying physiology, I became interested in medicine. Upon graduation, I went to Ann Arbor, University of Michigan for my medical education. After that, I moved to Henry Ford Hospital for my residency training before going to and completing my fellowship training at the Beth Israel Deaconess Medical Center.
 An
An 

 A urologist can prescribe medication to reduce the symptoms of an enlarged prostate and also to control the enlargement. The available medications include:
A urologist can prescribe medication to reduce the symptoms of an enlarged prostate and also to control the enlargement. The available medications include: